Table of Contents
Clinical Case scenario:
A 52-year old male patient got admitted to the medical ward complaining of sudden onset weakness and numbness in his lower limbs which has progressively increased over the past two weeks. Initially, the weakness has been in the leg muscles and the foot, but it seemed to be gradually ascending proximally. He also complained of back pain.
He did not have weakness in the arms, facial muscles or any breathing difficulties at the time of presentation.
He also gave a history of an upper respiratory tract infection a couple of weeks back that had settled in a few days after taking over the counter medications.
What could be his medical condition? How can we arrive at a diagnosis? Let’s break down the clinical scenario step by step to find out.
Differential Diagnosis (DDx) We Had in Mind
Given the presenting symptoms, we soon realized this could be some form of polyneuropathy. Here’s a list of differential diagnosis we had in mind at the time.
DDx:
- Guillain Barre Syndrome (GBS)
- Chronic inflammatory demyelinating polyradiculoneuropathy
- Idiopathic sensory neuropathy
- Metabolic Neuropathy
- Toxic neuropathy
- Spinal cord compression
- Multiple Sclerosis
- Vitamin-deficiency neuropathy
But after analyzing the initial symptoms, given the condition’s sudden onset, progressive nature, and the past history of infection, we felt that the condition was more likely to be GBS. However, we needed examination and investigation findings to come to a final diagnosis and to proceed with a management plan.
What is Guillain Barre Syndrome?
GBS is a very rare neurological disorder that can cause sudden onset muscle weakness, loss of sensations and sometimes even death. It is also called acute inflammatory demyelinating polyradiculoneuropathy (AIDP).
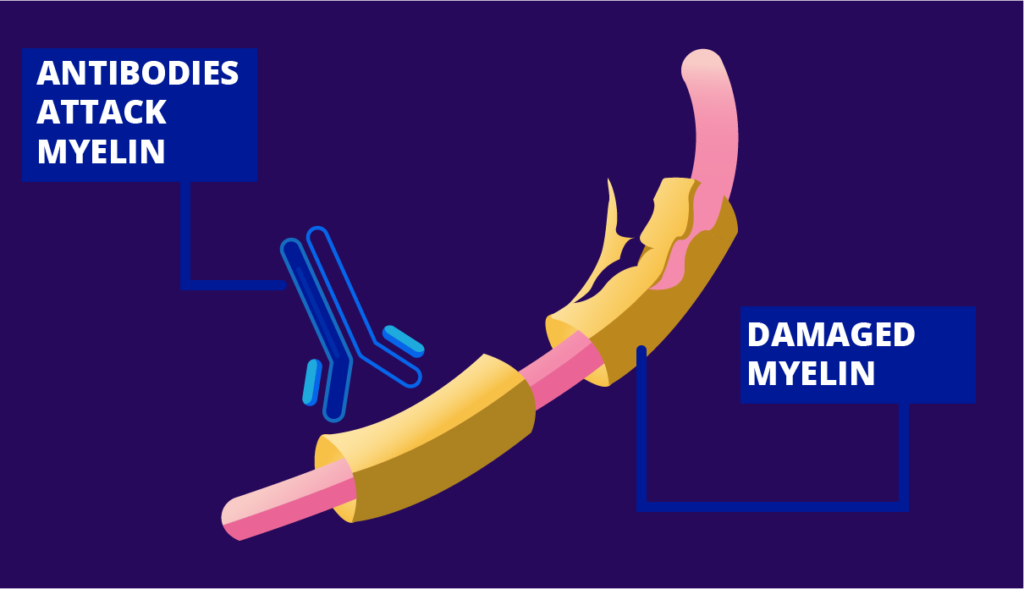
This condition occurs when our own immune system starts to attack nerves in the peripheral nervous system of the body by mistake. This happens usually after a period of infection, mostly by campylobacter jejuni and cytomegalovirus like pathogens.
The immune system gets deceived by the uncanny resemblance between homologous epitopes of the microorganism’s liposaccharides and the patient’s nerve gangliosides (of myelin sheath) and it starts attacking one of its own kind. As a result, the nerves get demyelinated giving rise to symptoms like muscle weakness/paralysis and loss of sensation.(1)
Findings we wanted to elicit on clinical examination
- Symmetrically reduced muscle power in both lower limbs (weakness is ascending and progressive in nature)
- Numbness and reduced sensation in the limbs
- Absent or reduced tendon reflexes
- Reduced power in the bilateral upper limbs if the disease has progressed proximally.
- Signs of cranial nerve involvement such as facial droop, dysarthria, dysphagia, and pupillary changes.
- Ophthalmoplegia (paralysis or weakness of eye muscles) and ataxia [signs of a rare, proximal variant of GBS called the Miller-Fisher syndrome]
- Autonomic findings like tachycardia/bradycardia, orthostatic hypotension, anhidrosis and/or diaphoresis indicate damage to the sympathetic and parasympathetic nervous system.
- Increased respiratory rate and dyspnea can occur when respiratory muscles are affected.
What are the investigations we ordered?
Initial investigations included the basic investigations like;
- Full Blood Count (FBC)
- Erythrocyte Sedimentation Rate
- Urine Full Report
The other investigations we ordered include;
- A nerve conduction study (NCS)
- Electromyography (EMG)
- Lumbar Puncture for CSF proteins
- Pulmonary function tests- Spirometry
- MRI and CT spine (kept as the second-line investigation options)
How we arrived at a diagnosis
Our suspicion on clinical grounds could be confirmed by the investigation findings.
- GBS results in abnormal nerve conduction study results. They include;
- Reduced nerve conduction velocities
- Prolonged distal motor latency
- Conduction block
- Temporal dispersion of waveforms
- Prolonged or absent F waves
- Findings of the CSF study may include;
- Raised CSF protein levels; usually up to 1-3g/L (indicate the widespread inflammation of the nerve roots)
- Normal white cell count
- Normal glucose level
- Electromyography (EMG) usually shows no change in acute nerve lesions, but may develop fibrillation in 3-4 weeks.
- If the respiratory muscles are also affected, the spirometry results can be abnormal. For example, the reduction in the forced expiratory volume in one second (FEV1) may indicate restriction in expiration capability and respiratory muscle weakness.
- Magnetic resonance imaging (MRI) and computed tomography (CT) scanning of the spine can be utilized to exclude other possible pathologies of the spine.
- The presence of antibodies against GQ1b (ganglioside) may indicate the Miller-Fisher syndrome variant of GBS with a sensitivity of 90%.
Putting together the presenting symptoms, clinical examination findings and the investigation findings, a diagnosis of GBS can be made.
How can we treat a patient with GBS? It’s time to find out!
The management plan we adopted for the acute management of GBS
There is the risk of muscle weakness or paralysis spreading within hours or days to the respiratory muscles, compromising respiration. The patient may even need ventilatory support.
Therefore, it is crucial to monitor the ventilation (vital capacity) of the patient regularly in order to detect the slightest changes as quickly as possible. If respiratory failure occurs, mechanical ventilation should be carried out.
In order to prevent deep vein thrombosis due to immobility, the patient can be given low-molecular-weight heparin and compression stockings to wear.
The main goal of treating GBS is to prevent further nerve damage. Currently, two main treatment modalities can be adopted for acute management.
1. Intravenous immunoglobulin Therapy
This includes giving immunoglobulins as intravenous injections. To reduce the severity and duration of paralysis, immunoglobulins should be given within the first two weeks of the disease.
Immunoglobulins are the body’s natural defence molecules battling infections. When they are given intravenously, they induce a dilution effect on the harmful antibodies attacking the nervous system.
Furthermore, the antibodies given externally go and attack the trouble-making antibodies and remove them out of the picture. This leads to better and fast recovery rates in GBS.
However, the patient should be screened for IgA deficiency before giving the immunoglobulin therapy as individuals with congenital IgA deficiency have a tendency to develop severe allergic reactions due to IgG antibodies.
2. Plasma Exchange
This method includes removing harmful antibodies that damage the nerves via an external catheter inserted through a vein. Usually, the harmful antibodies are present in the plasma component of the blood. Here, the plasma component is replaced and the blood cells are returned back into the body.
The plasma exchange process also reduces the duration and severity of GBS.
Plasma exchange can be performed as an alternative treatment modality for immunoglobulin therapy. In normal clinical practice, either one of the techniques are performed at a time and not both at the same time.
The Miller-Fisher variant of GBS also can be treated with immunoglobulin therapy and plasma exchange.
How can we manage a GBS patient in the long-term?
The long-term management and follow-up plan for a GBS patient must include an extensive rehabilitation program.
We must prepare the patient to resume his daily activities and return to his pre-illness life as early as possible. This preparation should be done both mentally and physically.
The rehabilitation program must focus on achieving two main targets.
- To reduce the burden of disability
- To support the reconditioning process
Here are a few steps we can adopt in the long-term management of a GBS patient.
- Refer the patient to a rehabilitation program.
- Start graded physiotherapy
- Muscle-strengthening exercises (Active/passive)
- Range of motion exercises for joints (Active/active assisted/passive)
- Low resistance exercises to improve endurance
- Ankle-foot orthosis to prevent plantar contractures
- Functional training
- Gait training
- Balance training
- Increasing coordination skills
- Progressive introduction to walking without aid
- Training to carry out Activities of Daily Living like getting dressed
- Pain Management
- Pain medications
- Transcutaneous electrical nerve stimulation
- Reassurance to overcome anxiety and psychological impact
Usually, the patient can be sent home after completing a 12-week rehabilitation program. Our goal is to bring him to a state where he can carry out his activities of daily living without any external assistance.
Psychological counselling can be given for both the patient and caregivers alike to help them get through the situation.
What would be the prognosis of our GBS patient?
GBS can be a shocking disease to anyone due to its rapid onset and the severity of symptoms. However, luckily enough, nearly 70% of patients with GBS can fully recover. Even patients with respiratory failure can survive with timely intervention using treatments and intensive unit care.
The recovery process can take from a couple of weeks to several months or even years. Some patients report improvement even after 2-years.
However, this disease condition can become deadly for about 5-8% of the affected. Nearly 30% can be left with some form of disability or another. They can complain of weakness even up to 3 years.(2)
Very rarely, relapse of muscle weakness with tingling sensation may happen in about 3% of individuals several years after the initial attack.
Luckily, our patient did not get any long-term complications. He was all back to normal within a couple of months!
Conclusion
So, here’s the gist of our discussion. When a patient comes to you with rapid-onset, proximally advancing muscle weakness/paralysis with or without other symptoms like loss of sensation, make sure to include GBS at the top of your differential diagnosis list. Your sharp clinical judgement at the right time will help save a person’s life!
References
1. Kumar and Clark’s Clinical Medicine – 9th Edition [Internet]. [cited 2021 Feb 13]. Available from: https://www.elsevier.com/books/kumar-and-clarks-clinical-medicine/kumar/978-0-7020-6601-6
2. Guillain-Barré Syndrome Fact Sheet | National Institute of Neurological Disorders and Stroke [Internet]. [cited 2021 Mar 14]. Available from: https://www.ninds.nih.gov/disorders/patient-caregiver-education/fact-sheets/guillain-barré-syndrome-fact-sheet
