Table of Contents
Case Presentation
A 25 years old Japanese man presented to the hospital with chest discomfort, palpitations & faintishness. His father had died in sleep from a sudden unexplained cardiac arrest. He was rushed to the nearest hospital, where an urgent ECG was taken. There were ST-segment elevations followed up by T inversions in the leads V1 & V2.
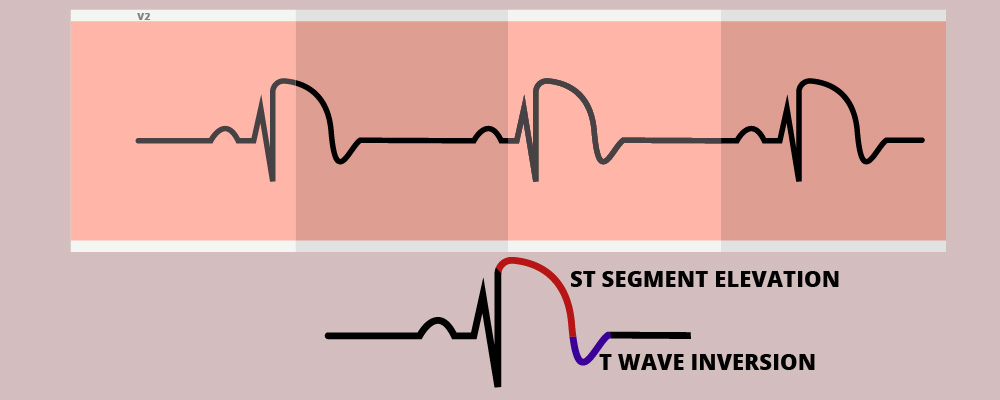
This finding is characteristic of Brugada Syndrome. A negative troponin test helped to rule out an acute ischemic event of the heart. The 2D echocardiogram study was normal. This is the classical presentation of patients with Brugada syndrome. They develop dangerous arrhythmias in the absence of structural heart diseases.
The electric instability of the heart can lead to sudden arrhythmias like Polymorphic ventricular tachycardia or Ventricular Fibrillation. Brugada syndrome is also known as sudden unexpected nocturnal death syndrome.
Pathophysiology of the channelopathy.
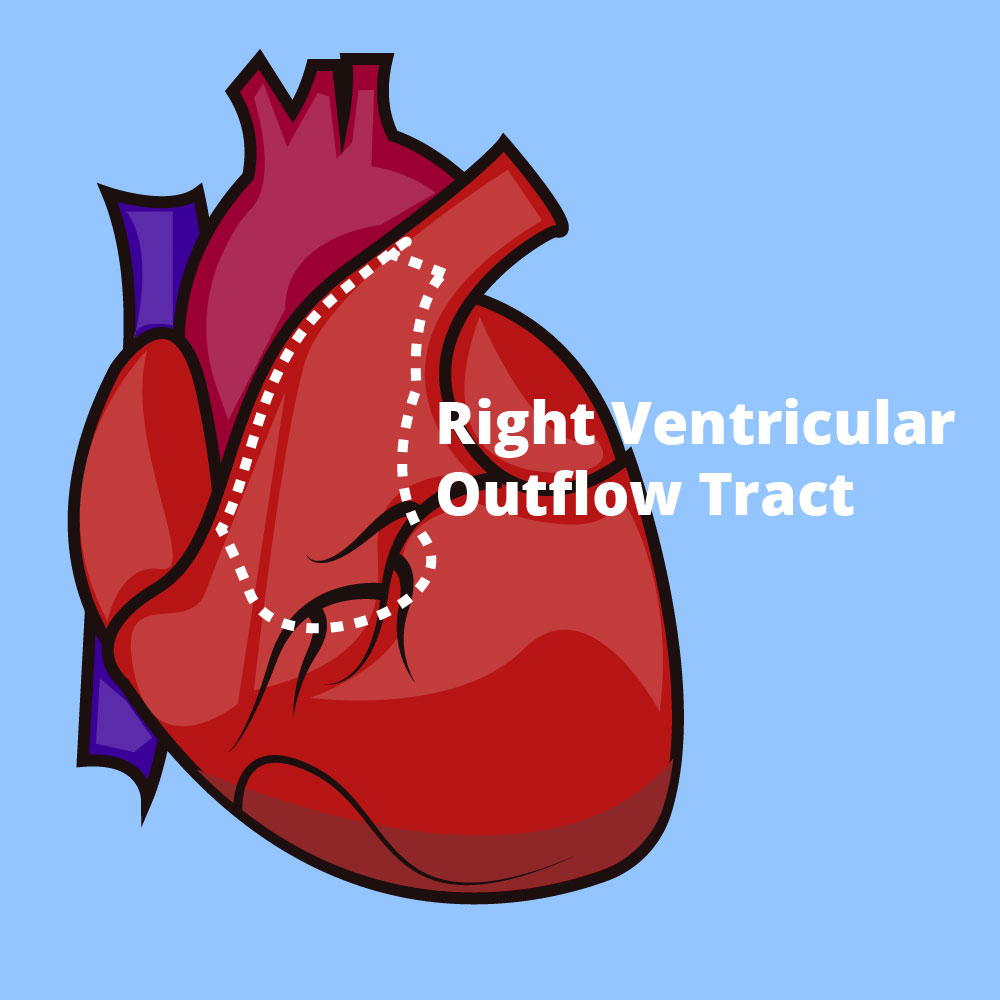
There are two main hypotheses for the Burgada Syndrome called Depolarizing and Repolarizing hypotheses. Both of them involve the Right Ventricular outflow tract (RVOT) area of the heart & have complex mechanisms. Let me try to simplify the “depolarizing hypothesis” for you.
Depolarization Hypothesis.
In Brugada Syndrome, there are abnormal Sodium channels in the epicardial portion of the right ventricular outflow tract of the heart. Depolarization occurs slowly in the epicardium compared to the myocardium & endocardium.
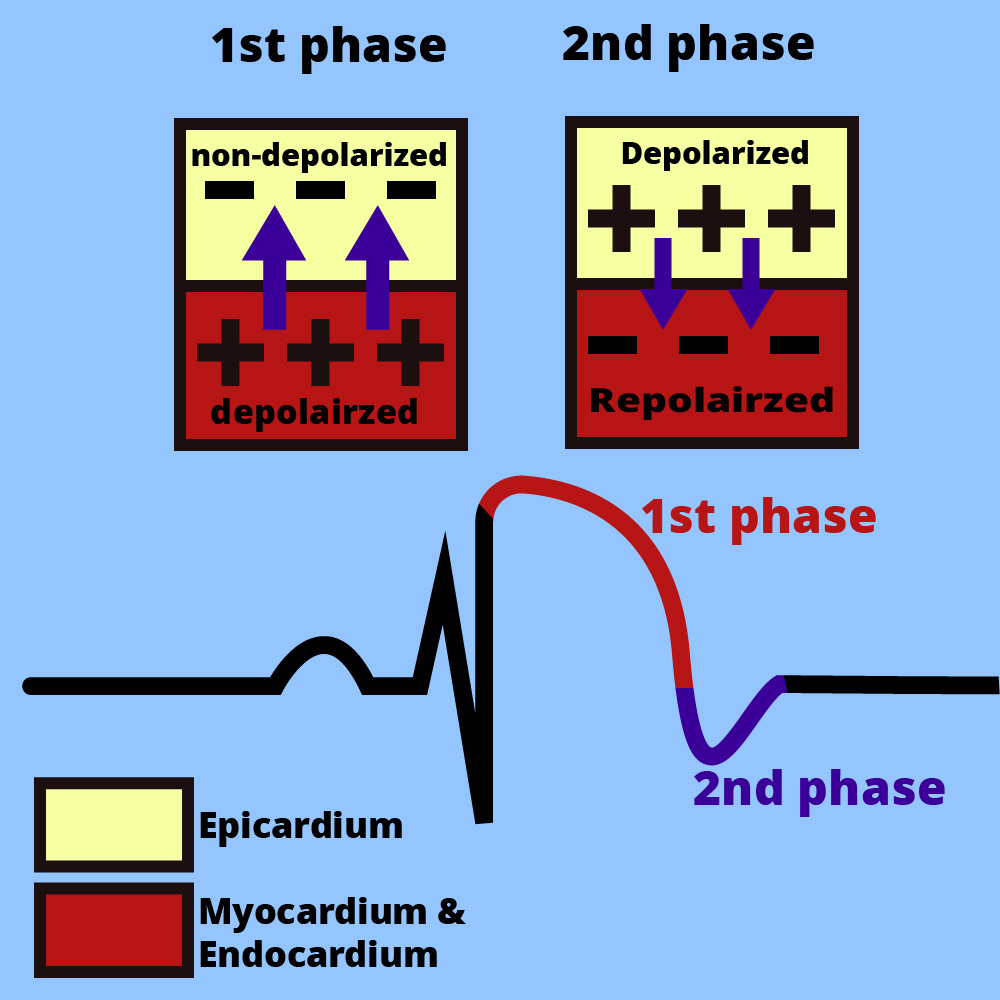
In the first phase, current flows from the myocardium to the epicardium due to the depolarization delay of the epicardium. This is reflected as ST elevations in leads V1, V2 & V3.
By the time the epicardium is depolarized, the myocardium & endocardium have already reached repolarization. This is the basis behind the T inversion during the second phase.
ECG patterns.
There are three distinct ECG variations in Brugada syndrome.
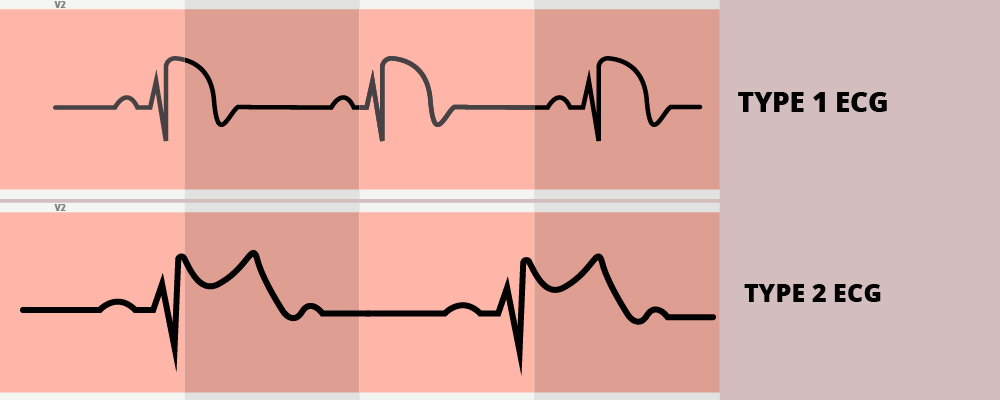
- Type 1: Coved type ST elevations followed up by T inversions in leads V1-V3. The ST elevations should measure above 2mm.
- Type 2: Saddle type ST elevations followed up by upright or biphasic T waves in leads V1-V3. Again the ST elevations should measure above 2mm.
- Type 3: Either type 1 or type 2 pattern with <2mm ST elevations.
Risk Factors
- Genetics: The gene responsible for abnormal sodium channels is SCN5. The allele responsible for the disease is autosomal dominant, meaning that it can override the effect of the normal allele. If a parent has this disease, there’s a 50% chance for their kids to get the disorder.
- Schizophrenia
- Class I antiarrhythmic drugs (eg: Flecainide)
Brugada Pattern Vs Brugada Syndrome
Sometimes we find Brugada pattern ECGs incidentally. It is called the Brugada pattern & doesn’t need any active interventions unless they are strong indications. For the brugada pattern ECG to be labeled as Brugada Syndrome, there should be at least ONE of the followings.
- Positive Family history
- of sudden cardiac death at <45 years of age.
- Coved type ECG
- Documented Cardiac Event.
- An episode of Ventricular Fibrillation (VF) or Polymorphic Ventricular Tachycardia (PVT).
- Syncopal/ Presyncopal attacks
- Nocturnal Agonal Respiration.
Treatments
The treatment for high-risk patients is ICD implantation. ICDs can detect sudden arrhythmias and convert them to a normal rhythm by delivering electric shocks. Carefully chosen Antiarrhythmic drugs like amiodarone or quinidine can be prescribed if the patients have recurrent arrhythmias resulting in ICD shocks. Catheter ablation also can be considered in these patients.
Brugada Drugs
Doctors should be extremely careful in prescribing drugs to patients with Brugada syndrome. I have listed some of the major drugs (source: https://www.brugadadrugs.org/avoid/)
- Antiarrhythmic drugs
- Ajmaline
- Allapinin
- Ethacizin
- Flecainide
- Procainamide
- Propafenone
- Pilsicainide
- Psychotropic drugs
- Amitriptyline
- Nortriptyline
- Clomipramine
- Desipramine
- Lithium
- Loxapine
- Trifluoperazine
- Oxcarbazepine
- Anesthetic drugs
- Bupivacaine
- Procaine
- Propofol
- Other substances
- Acetylcholine
- Alcohol
- Cannabis
- Cocaine
- Ergonovine
