A snake bite, especially a venomous one, would be a nightmare to any of us. Let us consider the story of a boy who happened to have that experience first-hand. The worst part of his story is that snake was a highly poisonous cobra.
Table of Contents
Case Scenario
Ramesh, a 14-year-old schoolboy presented to our emergency unit with a history of a cobra bite on his right foot two hours ago. He had been playing in the woods with his friends when he had felt a sudden pain in his right foot and noticed a cobra crawling near him.
His pain at the bite site was unbearable. His worried parents, who were accompanying him, mentioned that the swelling on his foot has been progressive with time. There was a fang mark on the dorsum of his right foot. He was conscious and oriented but had generalized abdominal pain and passed loose stools.
After admission, he developed difficulty talking and complained about both eyelids’ heaviness and difficulty opening his eyes. His pulse rate was 90 beats per minute and regular, blood pressure was normal, and his respiratory rate was 18 breaths per minute. There was no pallor or petechial rashes.
The attending medical management team was a little worried about his condition. Let us dive a little into Ramesh’s case to see why we should worry about a cobra bite and how to handle it in the best way.
Is Cobra a Venomous Snake?
Not all snake bites cause serious complications. But cobra is a venomous snake included in the Elapidae family. According to WHO classification, cobra comes under category one—snakes of highest medical importance. They can cause tremendous disability, morbidity, and mortality.
Going through our short discussion about Ramesh’s case, you will understand why they have named cobra a highly venomous snake.
What is the Pathophysiology of a Cobra Bite?
A bite of a cobra can cause envenoming. Simply put, it is the development of different clinical features resulting from the effects of the venom. Some snake bites are dry bites without envenoming. So, a cobra bite can vary from no symptoms to be fatal. Effects of cobra venom also differ in subcategory species. Post and pre-synaptic neurotoxins are the clinically significant toxins in most species. Cardio toxins, enzyme toxins, and complement activation factors also can be included in cobra venom. So, the cobra envenoming is mainly neurotoxic and necrotic.
Cobra envenoming cause local effects due to included toxins. Non-specific systemic effects also can occur in cobra bites. These may not result due to the effects of venom but due to altered psychology. Cobra venom can cause coagulopathies in severe conditions mainly due to consumption coagulopathies. Only a few will get acute kidney injury following a cobra bite.
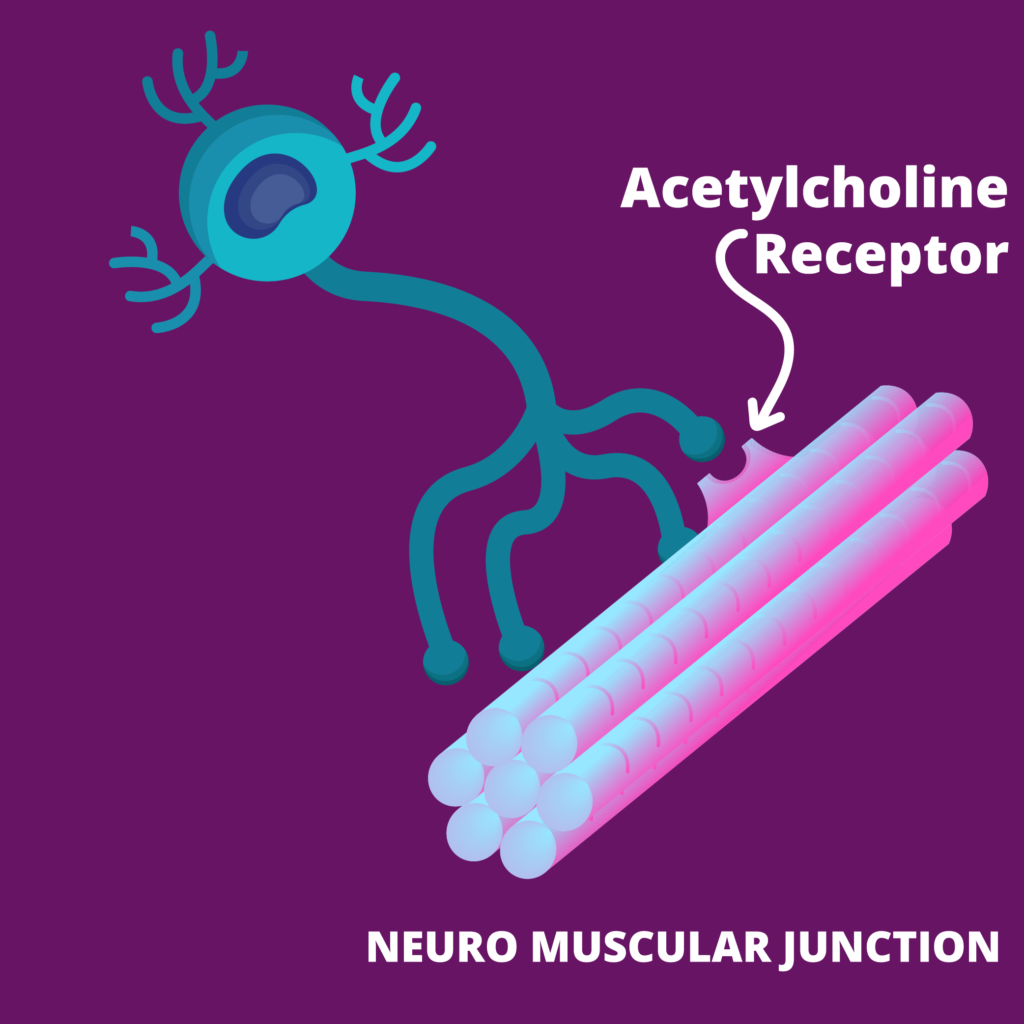
Neurotoxicity mainly occurs due to post-synaptic toxins. They bind to acetylcholine receptors and block synaptic transmission. Pre-synaptic toxins damage to the pre-synaptic membrane. Hope now you have gotten an idea of what has caused Ramesh’s clinical picture.
How Would These Patients Present?
Most of the patients seek medical care because they notice the snake bite. However, not all of them will develop envenoming features. In these cases, it is crucial to confirm whether the snake was really a cobra.
Some patients present with local effects like severe pain and swelling. Few may present with non-specific systemic effects—nausea, abdominal pain, vomiting, headache, or faintishness. Lymphadenopathy also can occur due to cobra venom.
Don’t forget that patients can also present with clinical features of neurotoxicity, including ptosis, difficulty in talking, external ophthalmoplegia, difficulty in swallowing, and limb weakness. Some can even present with respiratory distress due to respiratory muscle paralysis.
In cases like Ramesh’s story, it would be easy to pick it as a cobra bite. But some of these patients might not have noticed a snake bite. They may give a history of sudden pain while working in a paddy field or a bushy area.
What were Our Differential Diagnoses?
Even when a clinical encounter strongly suggests a specific condition, we must consider the other possibilities before starting treatment. Considering Ramesh, our main concern was that it is a cobra bite. But we thought about two other differentials which can give rise to the same clinical picture—Russell’s viper bite and hump-nosed viper bite. As we reiterated, the clinical picture of a cobra bite varies in a wide range. So, think accordingly and pick the best choice.
On Examination
What would you like to look for in Ramesh’s examination? Following airway, breathing, and circulation examination to ensure Ramesh’s condition is not life-threatening, we have to look into clinical features of cobra envenoming. The degree of local pain and swelling may vary from mild to severe. We have to assess the risk of developing compartment syndrome. Pain, swelling, and blistering at the site are seen in cobra bites and hump-nosed viper bites. Lymph node examination is important to assess lymphadenopathy.
Necrosis at the bite site can even lead to an amputation. So, we have to assess the spread of necrosis to the surrounding area. We should also assess his vitals and hydration status.
As Ramesh has already developed some neurological signs, we should do a complete neurological examination to elicit any other signs he may have. That will also give us a clue about his severity.
We can examine Ramesh for any bleeding manifestation which would suggest a coagulopathy. Coagulopathies occur more commonly in Russell’s viper bites and hump-nosed viper bites but is also seen in cobra bites in the severe stage. Hope you can see the clues given by examination to keep us on track to manage our patient.
What Investigations Should We Order?
How can investigations help Ramesh? We can use investigations to exclude our differentials, monitor progression, and identify any complications. We can do basic investigations—full blood count, blood picture, and SGOT. Lactate dehydrogenase and serum electrolytes also play an important role. Urine analysis for protein and hemoglobin can be done.
Considering imaging, we can do a chest x-ray to assess lung fields, abdominal USS to assess renal architecture and free fluid, and CT brain to exclude hemorrhage. We also can check creatine kinase for myotoxicity.
Whole blood clotting test, prothrombin time, activated partial thromboplastin time, and INR will give us an idea about coagulopathy. These can be prolonged due to disseminated intravascular coagulation or venom-induced consumption of coagulation factors.
How to Manage a Cobra Bite?
The most important thing is to seek medical assistance as soon as possible. You can try to photograph the snake, as it would help identify the snake.
First-aid for snake bites
It is essential that everyone know first-aid treatment for snake bites. The main rule is “do no harm.” Aims of first-aid are to delay the venom absorption, prevent complications, maintain airway, breathing, and circulation, and keep the patient safe until proper medical care is reached.
In a poisonous snake bite like a cobra bite, we are pressed for time. So, we have to attend to it quickly and call for help if needed. We can give basic life support, reassure the victim, wash the bite site well with water and soap, and immobilize. A crepe bandage and a splint are best for this.
Don’t forget to remove any rings or bangles. Swelling at the site will depend on the species, and cobra venom has a high risk of local effects. We have to remove constricting clothing as well. We should try to keep the patient as comfortable and warm as possible. These simple measures can save a victim’s life.
Don’ts in a Snake Bite
We should not exert pressure on the bite wound, tie a tourniquet near it, give alcohol or fruit juice, incise, suck, keep stones, or insufflate as they can add fuel to the fire.
You should never try to catch the snake. It is dangerous to handle a venomous snake, as even a decapitated head can cause envenoming. These have no benefit on the patient. They may put others in danger while the victim deteriorates.
Medical Management
Start with initial assessment and resuscitation. Check for local and systemic envenoming features. We should insert two wide-bore cannulas and withdraw blood for investigations. Keep medication ready for managing anaphylaxis. We have to give tetanus prophylaxis if needed.
Antivenom
If indicated, we can give antivenom treatment. Indications for antivenom treatment are any specific systemic envenoming, coagulopathy, neurotoxicity, myotoxicity, or more than half of the limb being affected by local effects of a cobra bite. Antivenom is the mainstay of treatment in a cobra bite with envenomation. As a cobra can deliver multiple bites in a single attack, antivenom dose will depend on the incident and the patient factors.
Most of the symptoms will ameliorate with the antivenom alone. Some symptoms will need both antivenom and supportive therapy to get corrected. So, we can give antivenom to Ramesh as he has developed neurotoxicity.
But there is a risk of anaphylaxis with antivenom. Prophylaxis administration of adrenaline reduces the rate of reactions. Facilities to manage anaphylaxis should be prepared before giving antivenom, and monitoring for the reactions should be done.
Supportive Therapy
We can give paracetamol or morphine to relieve his pain. But we must avoid NSAIDs as they can deteriorate his condition. Some patients may warrant antibiotics and fluid resuscitation.
To manage local necrosis, we may have to perform a surgical excision or amputation. Ventilation for respiratory paralysis and renal replacement therapy may be needed in severe conditions.
We have to continue monitoring for envenoming features. Monitoring vital signs, including pulse rate, respiratory rate, blood pressure, and oxygen saturation, is an essential step. We have to monitor his urine output too, as there is a risk of developing an acute kidney injury.
We may have to wake Ramesh and perform neurological examination every hour to ensure breathing and other neurological functions. We can’t afford to forget that Ramesh can develop a life-threatening complication at any time.
What is New Around the World
International organizations, mainly WHO, have renewed interest in snakebite envenoming. So, awareness, research efforts, and the development of new treatments have become a focus worldwide.
A new trend to identify the snake is genetic testing to determine the snake species by genetic analysis of swabs from the wound at the bite site.
Prognosis of a Cobra Bite
Most patients have a good prognosis without specific treatment. The good news is neurotoxic effects due to cobra venom can be completely reversible, though it takes some time.
So, Ramesh can have a totally normal life again. But, deaths due to cobra bites have been recorded, and the first two to six hours are crucial considering fatal events.
Permanent disabilities and psychological damages can occur in some people. Antivenom administration without delay with supportive therapy will reduce the risk of morbidity and mortality.
Follow-up Care
We have to follow up Ramesh to assess the long-term complications of the cobra bite and the antivenom. If residual neurological deficits are present, we may have to assess their progress with time.
Antivenom can cause serum sickness five to ten days after the treatment. They can develop fever, muscle aches, or joint swelling due to this. Last but not least, we have to educate our patients on how to prevent a snake bite in the future.
How to Prevent a Cobra Bite?
First, let us see how to identify a cobra. Cobra usually has a spatula-shaped head with an expandable hood. Characteristic spectacled mark at the dorsum of the hood helps to identify a cobra easily. Cobra has divided subcaudals, and there are two black patches in the ventral surface of the neck. So, if you see a snake with these features, go to safety at once. However, don’t forget that there are so many other poisonous snakes too.
Cobra bites are more common in tropical areas. Sub-Saharan Africa and South Asia show high mortality and morbidity due to cobra envenoming bites. Though it is rare, some cases are reported in the Western world among the reptile handlers in reptile parks.
It is of everyday importance to know how to prevent a snake bite. Minor factors like safety footwear, avoiding dangerous places, good light in the night, clear surroundings, and storing crops outside the house can do a massive job to save us from snake bites.
But we have to keep in mind that snakes are a part of nature, and there is no need to kill the snake and bring it to the medical care with the patient. Humans are only accidental victims. So, the best way to avoid a snake bite is to protect ourselves from exposing to a snake.
Conclusion
Cobra bite clinical picture varies from no clinical features to fatal conditions. We have to take any cobra bite seriously and encourage seeking immediate medical care. First-aid and early interventions are vital to reduce mortality and morbidity.
References
- Cobra envenomation (Robert N.L.et al)
https://emedicine.medscape.com/article/771918-overview
- Venomous snakes-CDC
https://www.cdc.gov/niosh/topics/snakes/default.html
- Snake bites- John Hopkins medicine
https://www.hopkinsmedicine.org/health/conditions-and-diseases/snake-bites
- First-aid for snake bites