We will discuss how diabetes can affect your vision, the prevention, diagnosis, and treatments. Most weight is given for Diabetic Retinopathy; but other Diabetic eye conditions are also explained in this article.
Table of Contents
How does Diabetes affect your eyes?
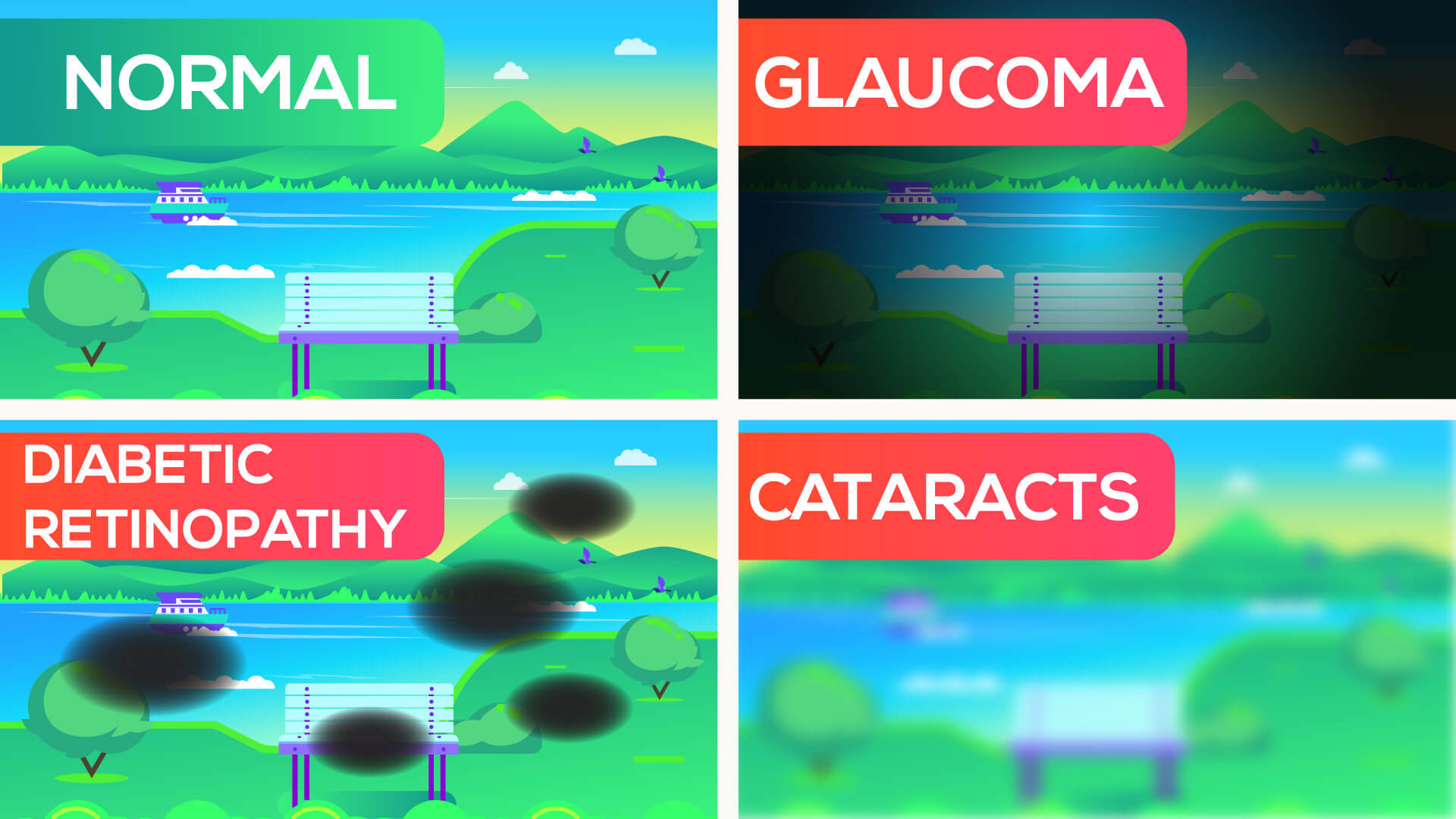
Diabetes affects the vision in many ways. Let’s begin the discussion with the least serious condition: Hyperglycemia induced blurred vision. Hyperglycemia is when you have high levels of blood glucose. It can cause swelling of the eye lens, which ultimately leads to blurry vision. This is only a temporary condition and can easily be reversed by lowering the blood glucose levels back to desired levels.
Moving on to the long term eye diseases, let’s learn about Diabetic retinopathy, Cataracts, glaucoma, and macular edema.
Diabetic Retinopathy
Light enters the eyes through the pupils, travels across the lens and lands on retina. Retina has the receptors that convert light waves into electric signals. The optic nerve carries these signals to the brain to create images. The retina has a rich blood supply to support this complex task.
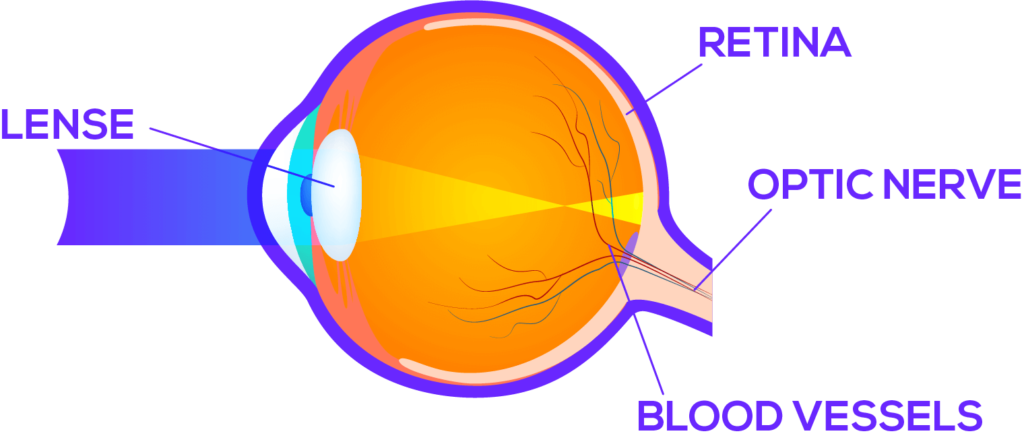
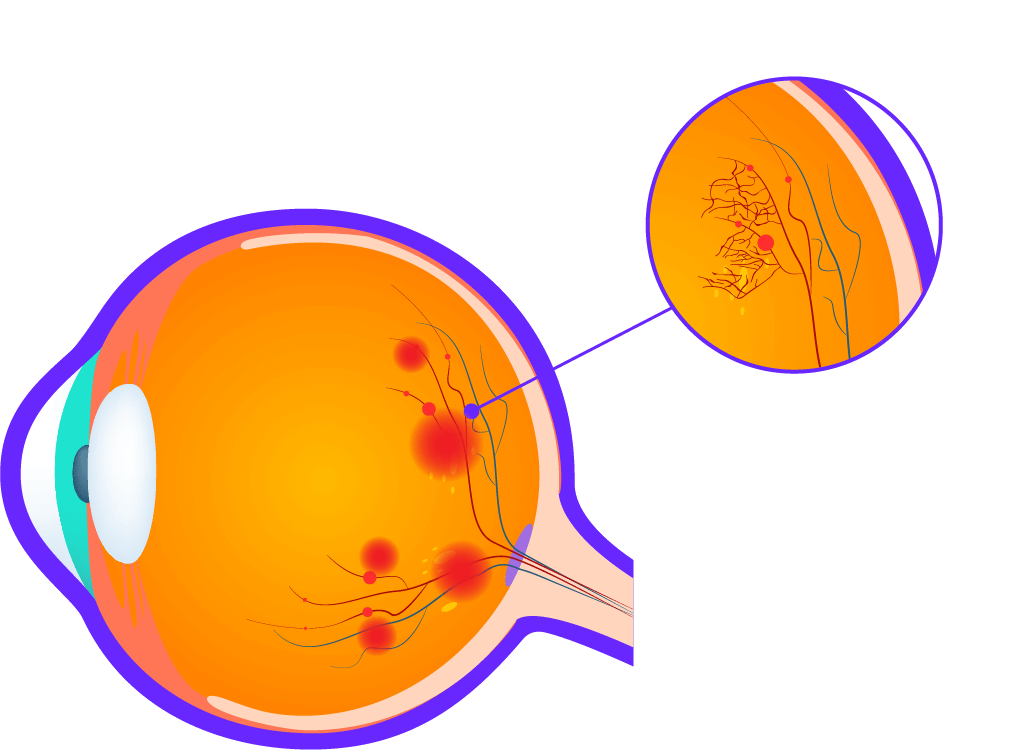
When you have diabetes for a long period, it can damage these blood vessels and cause defects in the retina. This condition is called diabetic retinopathy. It has three stages.
The first stage is called Diabetes without retinopathy.
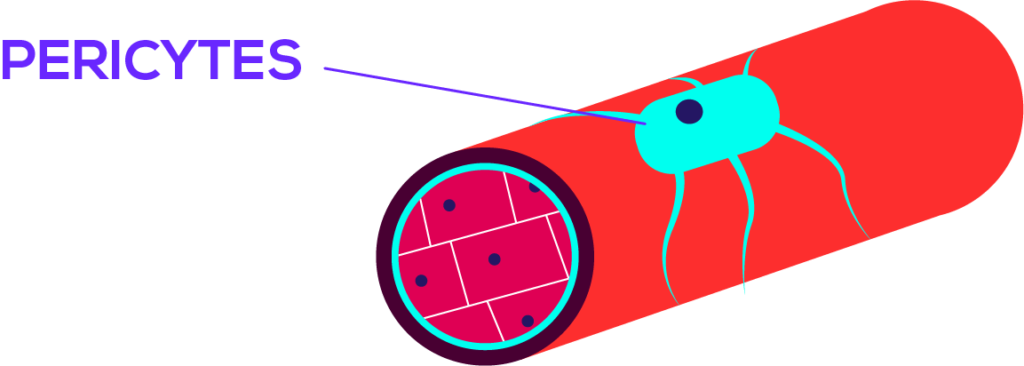
- The walls of micro blood vessels are covered by a type of cells called pericytes.
- In this first stage, pericytes of the retinal vessels are slowly damaged.
- But the retina will appear normal in eye examination and you will have no symptoms.
The second stage is called Non-Proliferative Retinopathy
- In this stage, without the support of pericytes, walls of retinal blood vessels bulge out creating microaneurysms. They appear as red dots in the retinal examination. When these microaneurisms rupture it gives rise to small blot and dot hemorrhages.
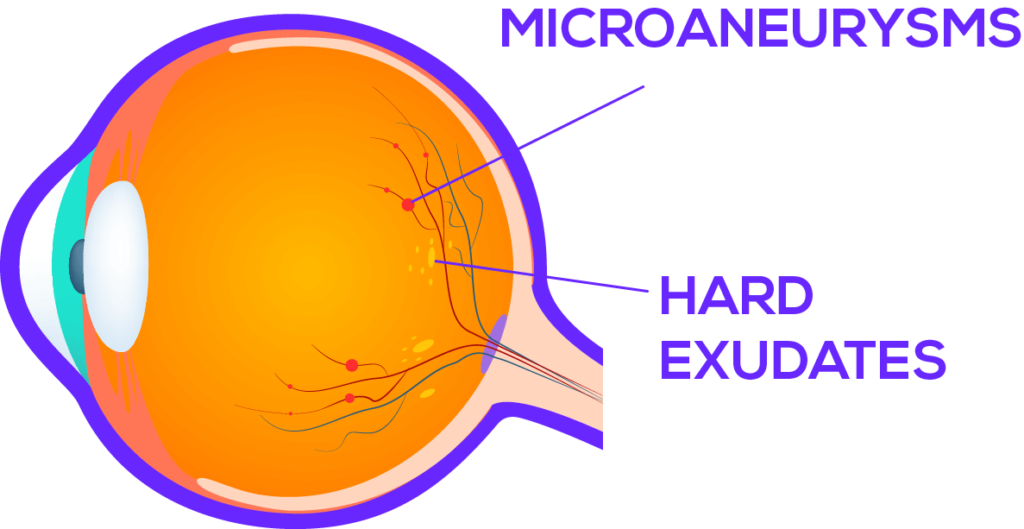
- Lipids and proteins will leak through the damaged vessel walls and collect within the retina as hard exudates.
- These hard exudates and Microcaneurisms characterize the Non-proliferative retinopathy stage. Micro aneurysms are considered as the first sign in diabetic retinopathy.
The third stage is called Proliferative retinopathy
- Due to the vessel damage, the retina is deprived of oxygen. Therefore it secretes a chemical called VEGF or Vascular Endothelial growth factors that stimulate new vessel formation. This new vessel formation is called neovascularization. But these new vessels are very fragile and can suddenly rupture and cause vitreous hemorrhages and retinal detachments.
- Therefore proliferative retinopathy is treated aggressively with a technique called photocoagulation, where laser rays are directed at retinal vessels to stop new vessel formation and to seal the leaking vessels.
- Non-proliferative retinopathy is treated with anti-Vascular endothelial growth factor injections (anti VGEF).
Diabetic Macular Oedema
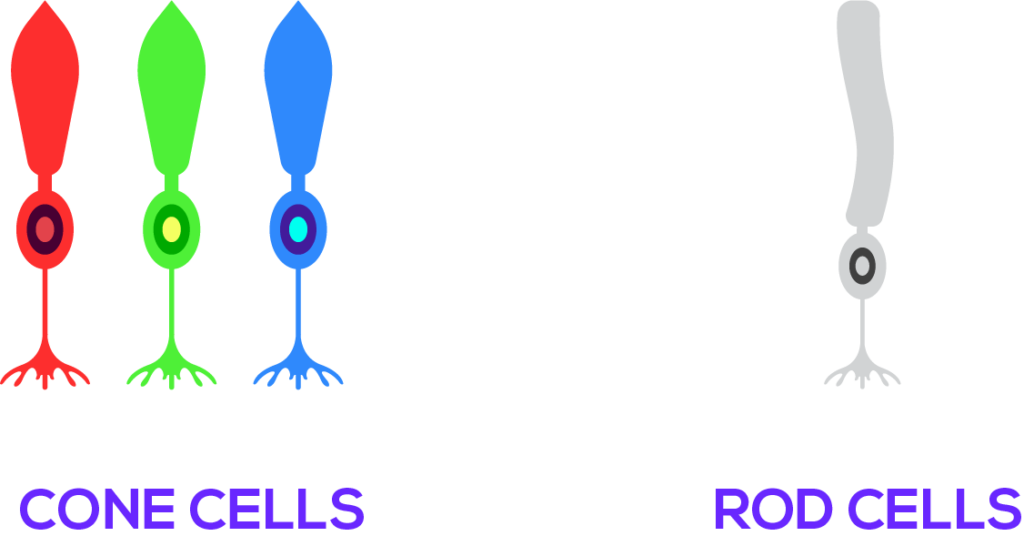
We already know that retina is a collection of light receptors. The macula is the part of the retina that contains a vast majority of specialized light receptors called “Cons”.
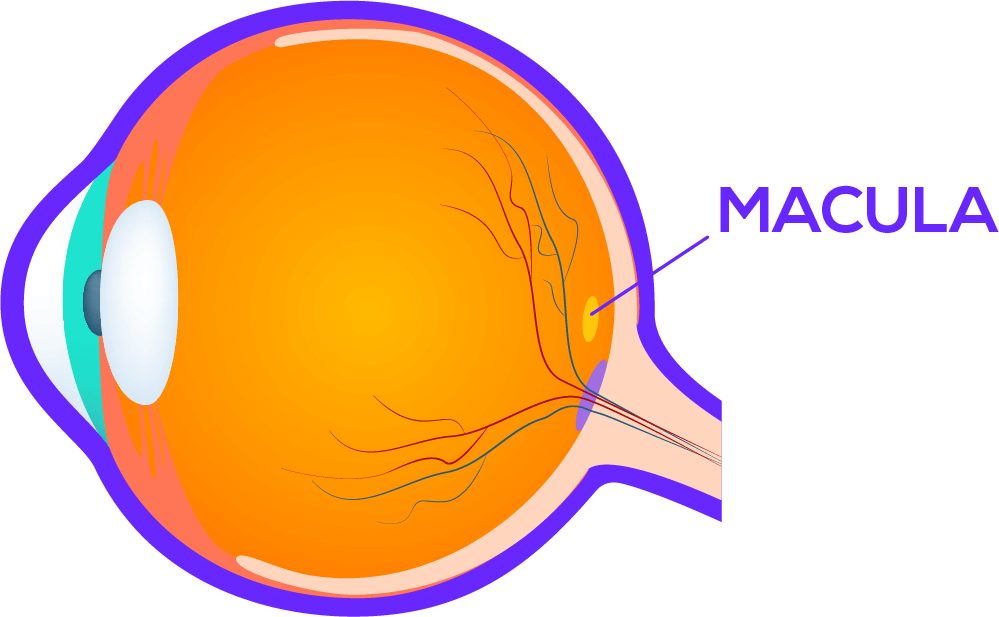
Cons are sensitive only for certain wavelengths of light, such as green, blue or red, a trait that grants the ability to differentiate colors.
Therefore macular is the part of the retina responsible for central, high resolution, colored vision. When you have leaky blood vessels due to diabetic retinopathy, fluid can accumulate in the macula and cause blurred vision with floaters. Macular edema is usually treated with photocoagulation.
Glaucoma
- The eye can be divided into two parts; the anterior segment and the posterior segment. They are filled with two different fluids named aqueous humor and vitreous humor.
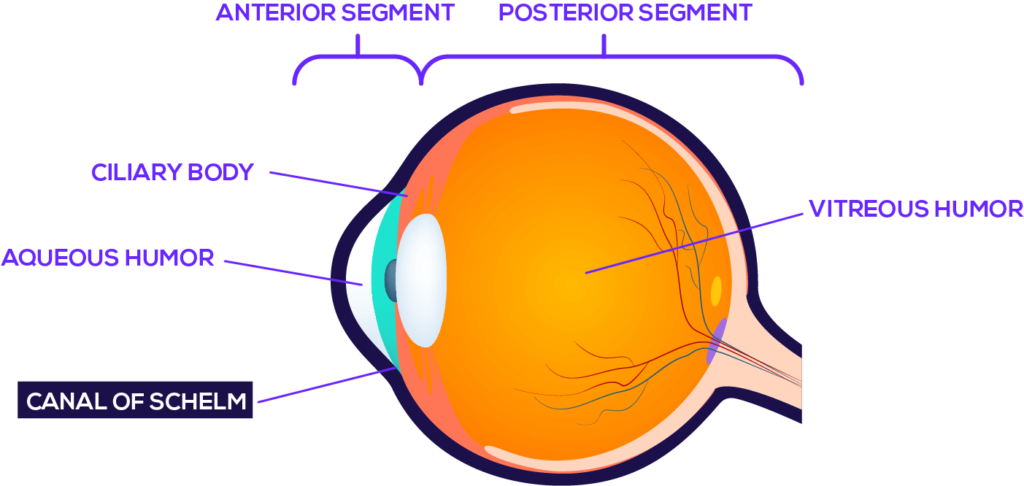
- Aqueous humor is secreted by the ciliary body and absorbed by a drainage system named the canal of schelm.
- If the canal of schelm is blocked for some reason, fluid gets accumulated and increases the pressure within the eye. This can damage the optic nerve and cause glaucoma which is characterized by peripheral vision loss.
- Diabetes increases the risk of developing a type of glaucoma called open-angle glaucoma.
- It can be treated with eye drops that decrease the aqueous humor production such as timolol which is a beta-blocker or using prostaglandin analogs such as bimatoprost or latanoprost which increases the outflow of aqueous humor.
Cataracts
The job of the eye lens is to focus the light beams onto the retina. To accomplish this task, a good functioning lens should be transparent.
Glucose is converted to a substance called Sorbitol in our body. The high osmotic properties of sorbitol can cause fluid accumulation within the tissues. To prevent this, sorbitol is broken down into fructose by an enzyme called sorbitol dehydrogenase.
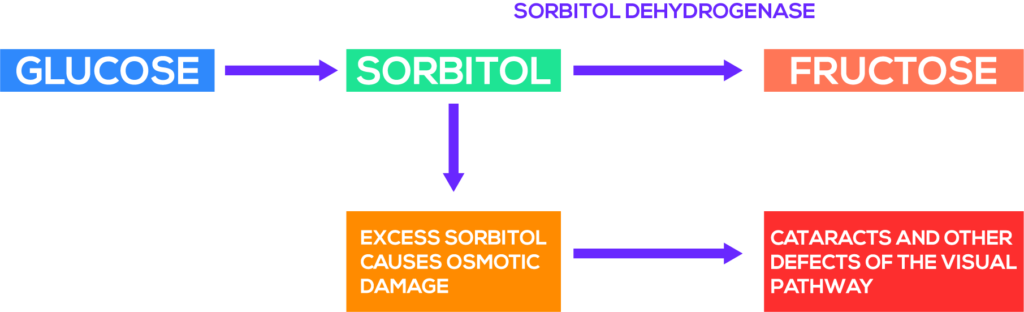
Unfortunately, our eye lens hasn’t got much of this enzyme to breakdown sorbitol. Therefore in people with high blood glucose levels, sorbitol is accumulated in the eye lens and makes it swollen and opaque like a white cloud.

Cataract surgery is the treatment option when it causes vision impairment.
Symptoms of Diabetic Eye Diseases
Blurry vision, dark areas in the visual field, poor color vision, peripheral vision loss or floaters are the typical symptoms. Though its rare, complete vision loss can also occur in diabetes.
How to diagnose diabetic Eye Diseases?
- Doctors perform a dilated eye exam to diagnose diabetic eye disease.
- First, your pupils will be dilated with eye drops.
- Then they will have a good look at your retinas through a magnifying lens to identify characteristic features.
- They will also use other tests such as visual acuity tests and tonometry to aid the diagnosis.
How often should you undergo eye examination?
Yearly eye examinations are recommended for people with diabetes. This yearly screening should start right after the diagnosis in patients with type 2 diabetes and within 5 years of diagnosis in patients with type 1 diabetes.
How can you prevent or control diabetic eye disease?
Controlling blood glucose levels is the best way to prevent and control diabetic eye disease. Blood pressure and cholesterol levels should be optimized. And if you are a smoker, quitting smoking will markedly slow down the progression of diabetic eye disease.