Table of Contents
Introduction
Have you ever played Statues? It’s a popular childhood game where the objective is to freeze and remain motionless. You move – your movement is detected – you’re out.
Imagine a darker version of this. A state of being where you are frozen against your will, and the detection of any minute movement you make could be your salvation.
Sounds frightening? It is.
Locked In Syndrome. This disorder resembles what was a source of fun in times past, but warped into a depressing source of hopelessness and sheer frustration.
Case Report:
A 52-year-old male was brought to the emergency care unit, unconscious, after having suffered – based on the bystander’s history and patient’s signs and symptoms – a stroke. He was immediately given ICU care, including being connected to a ventilator as his comatose condition continued.
Weeks went by with the patient showing no signs of waking, although the brain activity detected by a functional MRI (Magnetic Resonance Imaging) ruled out brain death. It was then that the possibility of a new diagnosis was brought up.
Locked In Syndrome
A patient may fall into a coma due to any one of many reasons. His family is grief-stricken, anxious, yet harbor hope that one day he may open his eyes again and rejoin the world of the waking. The family sits with him, reads to him, and holds his hand.
Waiting.
On the other side – the patient. He gradually awakens from a state of deep unconsciousness. Voices may reach him. Light may filter in through his eyelids. He can slowly realize that his loved ones are speaking to and watching over him. He hears them call his name and plead with him to wake up.
But he finds he cannot. His mind is with him, his body is not. He cannot even so much as twitch a finger to let them know he is right there, awake and alert.
He has no choice but to lay there, motionless, and voiceless.
Waiting.
The fear and helplessness arising with LIS
Locked In Syndrome (LIS) – also known as a pseudo-coma (not exclusive to Locked In Syndrome) – is an extremely rare state when a previously comatose patient wakes up in mind but not in body. Without the ability to control or move his body, the patient is, essentially, “locked in” his own body.
In the most severe and debilitating form of Locked In Syndrome the patient is entirely paralyzed, unable to even blink. In less severe cases, patients may retain the ability to open and close their eyelids, and to move their pupils, albeit in a restricted manner.
This means that a patient with LIS is simply a person frozen in body but aware in mind. If they are told a joke, they can feel amusement. If they hear voices of friends or family members, they can recognize it, can pinpoint who is saying what. If a song is played within their hearing range, they may enjoy the song, and may even recall the words of the song in their mind. If a relatively non-complex math question is posed to them, they may mentally come up with an answer. However, for all their mental perception, they will be unable to convey their feelings and emotions, and their ideas and opinions.
Clinical Presentation
Signs of Locked In Syndrome are detected in patients who are in a coma. The first of signs may be:
- Flickering of eyelids which can improve into full out blinking of eyes
- Late twitching of fingers or toes
- Intact cognitive function even with total paralysis
- Any other signs which display patient’s awareness some time after the onset of coma
Etiology
Locked In Syndrome is caused by lesions causing damage to the part of the brainstem called the pons.
Main causes:
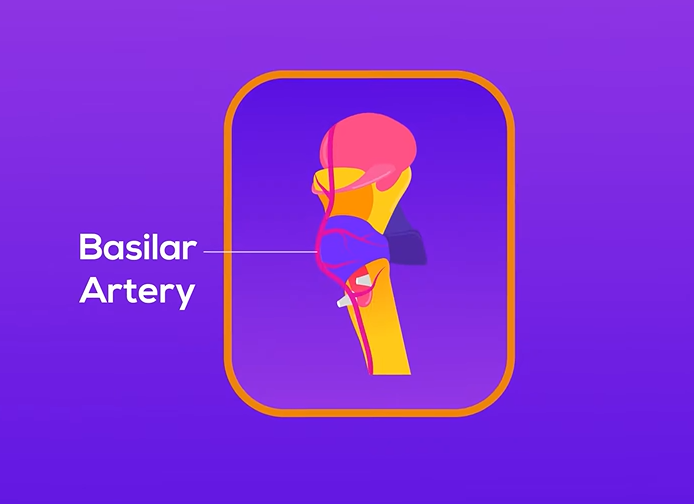
- Pontine hemorrhage – commonly occurs due to an occlusion in the basilar artery. (For example: a thrombus)
- Ischemic pontine strokes
- Trauma – injury to the pons
Less common causes:
- Tumors
- Infections
- Inappropriate drug use
Each of these causes neurons in the pons to degrade, either by ischemic infarction (Example: ischemic strokes) or by damage due to buildup of pressure within pons (Example: hemorrhages, tumors)
Pathophysiology
Locked In Syndrome is caused when the pons undergoes severe damage and neuronal necrosis, leading to paralysis.
Anatomy of the Pons
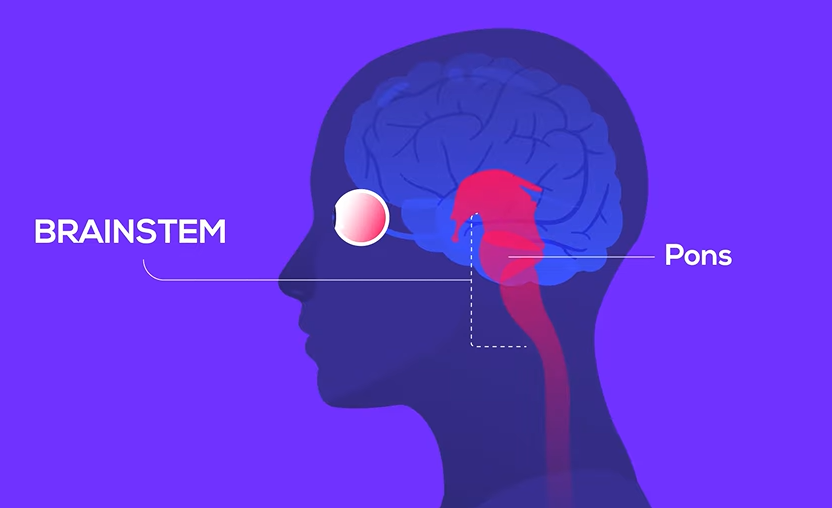
The pons is the second part of the brainstem, and it sits in between the midbrain and the medulla oblongata.
Most of its blood supply comes from the branches of the basilar arteries, called the pontine arteries.
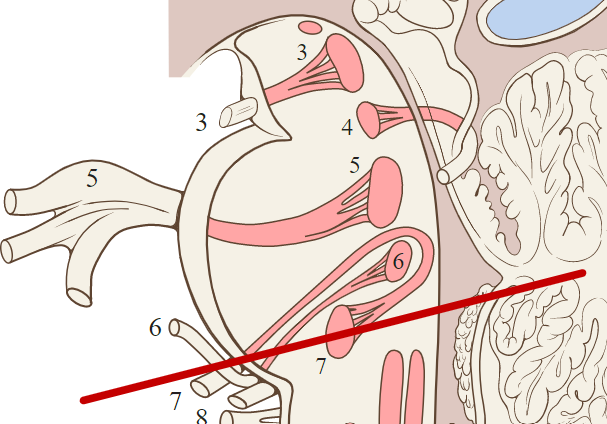
Four of the cranial nerves run over the anterior pontine surface:
- V – Trigeminal nerve – mainly transmits sensations from face (touch, pain, temperature) but also has a motor component to it
- VI – Abducens nerve – facilitates lateral movement of eyes
- VII – Facial nerve – carries sensation of part of the tongue, and innervates facial muscles (which give rise to facial expression)
- VIII – Vestibulocochlear nerve – facilitates balance as well as hearing
Pontine Functions
As part of the autonomic nervous system (ANS), the pons:
- Primarily transmits nerve fibers from cerebral cortex to cerebellum
- Contains nuclei which are partially responsible for respiratory regulation
- Regulates the sleep-wake cycle
- Includes the functions of the 4 cranial nerves running through (as mentioned above)
What happens when the Pons is Damaged?
Now that we’ve seen the anatomical and functional aspect of the pons, we can understand what goes on in the body when the pons suffers damage.
A patient with Locked In Syndrome is unable to carry out almost all voluntary muscle movements including:
- Lateral pupillary movements
- Moving their lips/mouth/jaw
- Chewing
- Speaking
- Swallowing
- Breathing (without ventilator support)
- Moving either of their arms or legs
- Hip flexion/extension
- Spinal motions
- Cranial nerve functions, in particular, the functions of the 4 nerves located in the pons, will be disrupted
- Impaired facial sensations, loss of control of facial expressions
- Side to side movement of eyes is no longer possible
- Impaired balance and hearing
Cognitive functions usually remain intact. Memory may be affected in some cases. The patient’s sleep-wake cycle also remains normal.
Categories of Locked In Syndrome
Locked In Syndrome can be divided into 3 categories based on the severity:
- Classic Locked In Syndrome – paralysis of all four limbs (quadriplegia) and incapability of speech (anarthria), with intact consciousness and vertical eye movements
- Incomplete Locked In Syndrome – same as above, with other voluntary movements in addition to vertical eye movements
- Total Locked In Syndrome – patient is completely immobile, cannot communicate in any manner, but is fully conscious behind closed eyelids
Progression of Locked In Syndrome
Several weeks after the patient sinks into a coma following an initial trigger (such as brain trauma or stroke), they may regain consciousness, but not the ability to move their body.
Diagnosis is considered in most cases whenever some sign of awareness is detected, most likely by a person who spends a large amount of time with the unmoving patient, usually a visiting family member or friend, or a frequent healthcare attendant.
Investigations
As soon as it is discovered that the patient is no longer unconscious, the patient is examined to confirm his awareness.
One of the leading signs is absent lateral pupillary movement but retained vertical pupillary movement.
Simply checking motor responses as included in the Glasgow Coma Scale (GCS) is not enough, since the diagnosis of Locked In Syndrome may be missed if eye movements are not carefully observed.
A Locked In Syndrome patient can understand commands and he still has the ability to blink, therefore voluntary vertical eye movements can be tested.
Brain Imaging – some of the most vital investigations for this diagnosis
- CT (Computerized Tomography) and / or MRI (Magnetic Resonance Imaging) – to visualize the pontine lesion causing LIS
- PET (Positron Emission Tomography), SPECT (Single Photon Emission Computed Tomography), Functional MRI (Magnetic Resonance Imaging) – to evaluate cerebral activity in order to confirm the preliminary diagnosis of Locked In Syndrome
- EEG (Electroencephalogram) – to monitor patient’s sleep-wake cycle (shows normal rhythm in Locked In Syndrome)
Management of Locked In Syndrome
- Maintain patient’s current health – ensure nutrition while preventing dehydration and starvation.
- Prevent further deterioration (Example: avoid infections by preventing bedsores)
- Stay vigilant for complications
Initially focus on underlying cause.
Example:
Basilar artery thrombus – use thrombolytics
Tumors – radiotherapy
Treatment of Locked In Syndrome
The most important course of action in improving patient’s condition is physiotherapy.
Extensive physiotherapy will be required to improve circulation and prevent spasticity due to the body remaining still for a long period of time.
In many cases of Locked In Syndrome, physiotherapy is one of the main contributors to any degree of recovery the patient can achieve.
Who Is at Risk of Locked In Syndrome?
Locked In Syndrome is rare, but among the cases that have been recorded, strokes are predominantly seen.
Therefore, patients who are at risk of developing strokes are in turn at risk of having Locked In Syndrome.
Around 1% of patients who suffer strokes have gone on to develop Locked In Syndrome.
Complications of Locked In Syndrome
Complications are largely due to the long duration of immobility of the patient caused by the extensive muscle paralysis.
- Aspiration pneumonia – due to patient aspirating the contents of the feeding tubes
- UTIs – via indwelling urinary catheters
- Thromboembolism – if patient does not receive physical therapy often enough
- More serious complications include respiratory failure and multi-system failure.
Difficulties Faced by Patients with Locked In Syndrome
- They need constant care and attention, as with any comatose patient.
- They cannot communicate easily – require special systems such as coding letters by blinking, or sophisticated methods like using computers to digitalize what the patient is trying to say.
- They are capable of very few and extremely limited movements.
- They cannot voluntarily breathe – they need the use of a ventilator.
- They cannot even swallow – a nasogastric tube must be inserted through the nostril down to the stomach in order to ensure the patient continues to receive adequate nutrition.
- They are incapable of sphincter control – measures such as indwelling urinary catheters are necessary
- With time and effective physiotherapy, the patient may show signs of recovery, but it is unlikely they will regain the ability to walk without support – an electronic wheelchair may be needed depending on the circumstances
Prognosis of Locked In Syndrome
Prognosis of Locked In Syndrome depends on:
- Etiology
- Age of patient
- Subsequent medical care afforded to the patient
Locked In Syndrome is not a death sentence in and of itself. But in cases of more severe forms of the disease such as Total or Classic Locked In Syndrome, some patients have been found to be depressed by their extremely poor quality of life and utter helplessness, that they lose the will to live.
When LIS is caused by disorders which are irreversible as well as progressive, such as pontine cancers, it is usually fatal.
Early diagnosis, thorough physiotherapy, and attentive medical care may help the patient to improve gradually but not completely.
Signs of good prognosis include –
- Regain of ability to move distal digits (fingers, toes) in tiny motions
- Horizontal eye movements within the first month of onset of coma
- Improved speech
- Improvement in swallowing
Mortality of Locked In Syndrome is highest during the first 6 months.
It has a 10-year survival rate of about 83%.
Did You Know?
Patients who have suffered from Locked In Syndrome have gone on to do remarkable things after their diagnosis. Many of them have managed to write books with the help of communicating devices, about the tragedy that befell them and their own thoughts and feelings about it.
For a patient who can use neither words nor hand gestures, to dictate an entire book by just blinking shows remarkable resilience and proves that while they may have lost much, including control over their own bodies, they have not lost their perseverance and willpower.
One such example is the French editor Jean-Dominique Bauby (1952-1997), whose stroke condemned him to suffer Locked In Syndrome, but who still went on to blink his one functional eye over ten months to eventually produce his book, The Diving Bell and the Butterfly, published in 1997.
Summary
Locked In Syndrome (LIS) is a rare but devastating disorder which leaves the patient in a state of full body paralysis but with their consciousness undamaged, effectively making them a prisoner in their own body. The condition can be triggered by many causes affecting the pons of the brain, the main cause being strokes. Close observation of the patient in the comatose stage along with neuroimaging are the most important and useful methods of diagnosis.
Some patients retain the ability to blink and, in some cases, minimally move their fingers and toes, and via physiotherapy and effective medical care, undergo a slow-paced improvement. However, complete recovery is not possible.
Communication is the greatest and most frustrating handicap these patients struggle with, but invention of codes with eye movements, and advanced computerized communication methods have enabled patients to get past the barrier of muscle paralysis-induced mutism, and even go on to amazing things like dictate their own books.
References
UpToDate:
https://www.uptodate.com/contents/locked-in-syndrome
thebmj:
https://www.bmj.com/content/330/7488/406.full
Physiopedia:
https://www.physio-pedia.com/Locked-In_Syndrome
Orphanet Journal of Rare Diseases:
https://ojrd.biomedcentral.com/articles/10.1186/s13023-015-0304-z
Wikipedia:
https://en.m.wikipedia.org/wiki/Jean-Dominique_Bauby
Image References:
“Locked In” following a stroke-induced coma – 123RF:
https://us.123rf.com/450wm/hofred/hofred2005/hofred200500104/147772367-intensive-care-doctor-examines-critical-woman-patient-receiving-oxygen-from-a-ventilation-in-intensi.jpg?ver=6
The fear and helplessness arising with LIS – Pinterest:https://i.pinimg.com/736x/53/46/da/5346da4a6268bd4d2231c368dbd0b71d–locked-in-syndrome-recovery.jpg
The brainstem – divided into the 3 major parts including the pons – Teach Me Anatomy:https://teachmeanatomy.info/wp-content/uploads/The-Parts-of-the-Brainstem-Midbrain-Pons-and-Medulla-600×420.jpg
The 4 cranial nerves within the pons: CN V, VI, VII, VIII – Lecturio:
https://cdn.lecturio.com/assets/Division-of-cranial-nerves-that-arise-in-brainstem.jpg
Glasgow Coma Scale – for evaluating level of consciousness in patients – First Aid For Free:
https://www.firstaidforfree.com/wp-content/uploads/2013/11/GCS.jpg
Brainstem glioma (pontine tumor) – Radiopaedia: https://prod-images-static.radiopaedia.org/images/23413/b740ddcd0e96cb1928682b04e83d84_gallery.jpeg
