Not all bacteria can survive an acidic environment. However, among those who can, there’s one that truly stands out. Helicobacter pylori or commonly known as H. pylori is famous for its ability to thrive in a rather harsh and acidic setting, the human stomach.
H. pylori has a closer relationship with human beings than one would imagine. Scientists believe that H. pylori (HP) resides in more than half of the human population. This minute trouble maker is responsible for causing gastritis in nearly 75% of people having the infection. It is also the main culprit behind more than 90% of ulcers in the duodenum and about 80% of ulcers in the stomach.
Long before the discovery of HP, people were having this misconception that it was only the food we ate, especially spicy food, and stress like lifestyle factors could cause gastritis and peptic ulcers. But with the discovery of HP in 1982 by two Australian doctors named Barry Marshall and Robin Warren this whole perception regarding gastritis was challenged.
These two scientists went to extremes in making this groundbreaking scientific discovery, so much so that Dr. Marshall ingested the bacterium himself to get the infection.
Not only that, he also went through a series of invasive procedures to prove his point to the scientific community. Prior to his bold act, he underwent a gastric biopsy to establish he didn’t have the infection at the time of self-ingestion. A while after drinking the medium containing bacteria, he started experiencing symptoms of gastritis. With the help of a repeat biopsy which contained evidence of a HP colony in it , he was able to prove his point at the end.
A lot of determination and self-sacrifice was behind this entire process. Later both scientists received the recognition they deserved and it was indeed a discovery worthy of the Nobel Prize!
Table of Contents
H. pylori- A survivor amidst adversity
Helicobacter pylori is a spiral-shaped gram-negative bacterium. It has multiple flagella which allows it to move about freely in the stomach.
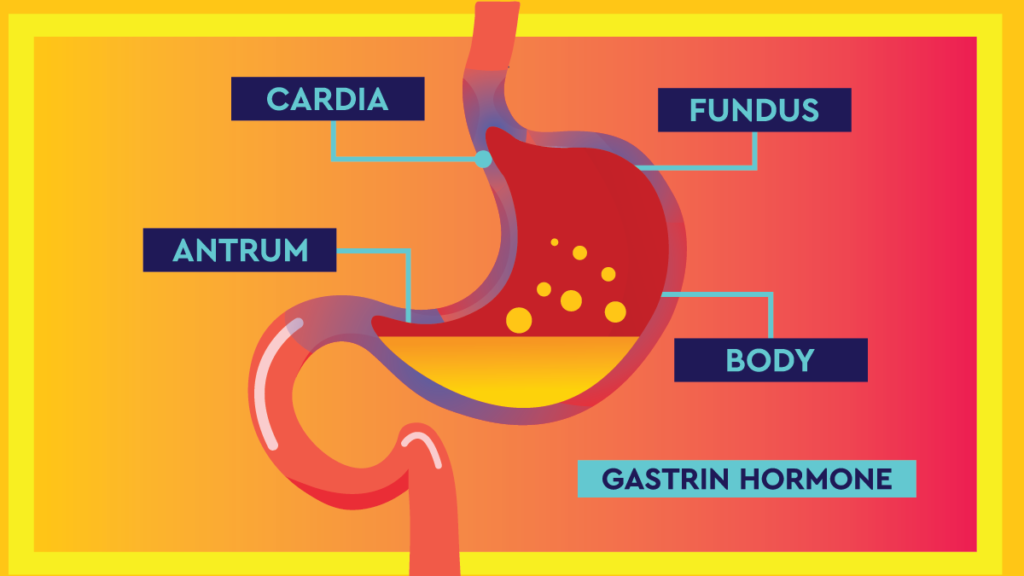
HP has a few tricks up its sleeves that allows it to thrive in a rather challenging, acidic environment like the human stomach. For starters, it lives in the mucus lining of the stomach, mainly in the antrum, where there is less acidity. It also produces a special enzyme called Urease, which can convert urea into ammonia. Urease neutralizes the acidic pH around the bacterium.
Once HP attaches to the epithelial cells and starts releasing enzymes which are lethal to the epithelial cells. As a result, inflammation of the gastric mucosa starts to set in. This finally gives rise to symptoms of gastritis, and if the condition is worse, even to gastric sores.
Symptoms
The most common complaint of individuals having HP infection is burning-type of epigastric pain. In addition, nausea and vomiting often accompany this pain. Loss of appetite and weight loss might also occur depending on the situation.

Diagnosis
Urease breath test is a quick and reliable way of diagnosing HP. Furthermore, methods like testing for antigens in stool samples, culture and histology of stomach biopsy samples, and testing for antibodies in the blood are also carried out.
Treatment
The main target of treating HP is to destroy the bacteria causing it. For this purpose, different combinations of antibiotics are used. Sometimes with addition of other drugs more effective treatment regimens are created.
Triple Therapy
Even today, the most classical, not to mention the gold standard method of treating HP remains the triple therapy. It involves combining two antibiotics with another type of drugs called, a proton-pump inhibitor, a medication which reduces acidity in the stomach. Clarithromycin is often combined with either amoxicillin or metronidazole as the antibiotic component of the therapy. This treatment is usually given for a duration of two weeks to get best results.
Antibiotic resistance
Using antibiotics as the key treatment modality is not without its shortcomings. Antibiotic resistance is one of the greatest challenges we face today. Improper usage, not adhering to the treatment protocols and discontinuing treatment before the recommended duration are the main reasons behind developing resistance.
With the discovery of several resistant bacterial strains spread all across the globe, the situation has become much grave. Resistance against clarithromycin and metronidazole is not that uncommon now.
Antibiotic resistance varies from region to region as well as from an individual to another. As a result, scientists try altering drug regimens with different combinations of medications to suit different circumstances. So, the best option is to identify the regimen that suits each and individual scenario and use it accordingly.
Levofloxacin-Based Therapy
Levofloxacin, a broad-spectrum antibiotic that belongs to the Quinolone category is now in use as a substitute for Clarithromycin in the triple therapy, mostly as the last resort. It has shown promising results, when given for a duration of 14 days. Sitafloxacin, a fourth-generation quinolone is also popular among practitioners in many regions. However, quinolones are not an exception for the problem of antibiotic resistance as resistant strains are emerging across the globe.
Bismuth Quadruple Therapy
While searching for alternative ways to treat resistant HP strains, scientists have come across Bismuth, a chemical element with the atomic number of 83, as a potential option. Bismuth is not something new for treating diseases. It has also been used in the treatments of wound infections, syphilis, and colitis for a very long time.
Scientific data shows that Bismuth lowers the pH buffering ability of HP. As a result, HP loses its ability to thrive in an acidic environment and gets destroyed eventually. In addition, Bismuth lowers HP’s defenses against oxidative stress and also reduces its ability to get attached to host cells.
According to scientific data, Bismuth alone is capable of destroying HP 16-20% of the times. Furthermore, Bismuth together with the triple therapy adds an extra 30-40% of success in the eradication process of resistant strains.
Bismuth Quadruple therapy involves making use of a regimen of two antibiotics along with Bismuth and a PPI for a duration of two weeks. It is mostly used in cases where Clarithromycin resistance is seen. The two anti-biotics can be either metronidazole and tetracycline or even amoxicillin and clarithromycin.
All-in-one built-in single capsule is also available at the moment. It has Bismuth along with metronidazole, and tetracycline (BMT).
This treatment has shown so much promise that, now it is used as the first-line treatment regimen for HP in many parts of the world.
Sequential Therapy
This regimen uses similar antibiotics as in others, but they are given in a sequential manner. First, a PPI is given along with amoxicillin for five days and is followed by a combination of PPI, clarithromycin and amoxicillin for another five days.
Amoxicillin is given first as it disrupts the bacterial cell wall ensuring other antibiotics that have entered the cell will stay inside and not leave though efflux channels in the wall.
Scientific data shows that the sequential therapy has a greater success rate more than the standard triple therapy.
Hybrid therapy
This regimen includes treating seven days with PPI and Amoxicillin, followed by another seven days of combined clarithromycin, metronidazole, amoxicillin, and PPI treatment.
Dual Therapy
High doses of amoxicillin along with PPI are used for two weeks in this regimen. It is simple as it has only two drug components. People are more compliant with this therapy as it is easier to take just a lesser number of pills. Despite its simplicity, it is very effective in eradicating HP.
Vonoprazan
Vonoprazan is a recently discovered medication similar to PPI and it also contributes to reducing gastric acidity. Vonoprazan is a reversible H+-K+ ATPase inhibitor and it is taken orally. Scientific data shows that it is a hundred times more potent, faster and have a longer-lasting effect than a regular PPI. Japan was the first country to use the medication in a clinical setting. However, it is still not approved in a lot of regions in the world.
Probiotics
HP is a tough organism to bring down with its ever-increasing resistance to treatment. It constantly changes battle strategies and develops ways to survive irrespective of the type of antibiotic used. Therefore, the help of an inside man will come in quite handy in a situation like this.
There exists a group of microorganisms, when administered in adequate quantities can contribute to restoring balance in the human digestive tract bringing about positive health outcomes. They reduce the risk of infections, cardiovascular diseases, and cancer while improving the overall health in the host. These microorganisms are also known as probiotics.
Lactobacillus and Bifidobacterium are two such bacteria commonly found in the human body. They compete with HP for mucosal adhesion, produce toxic substances and trigger immunologic response against HP in the body. When used in combination with the standard therapy, probiotics increase the overall HP eradication rate. Besides, they play a role in reducing the side-effects caused by other medications as well.
Anti- H. pylori compounds
Scientists are trying to develop chemical compounds that can target and attack crucial elements inside the HP bacteria while destroying them in the process. Most of these compounds target proteins in bacteria. They affect bacterial metabolism and demonstrate bactericidal effects. The main target of using them is to provide additional support to antibiotics and destroy the pathogens more efficiently.
Phytomedicine
This is an organic way of treating HP infection where herbal extracts are used instead of artificial chemical compounds. Scientists have taken a page out of the traditional Chinese folk medicine in developing these medications. They are looking into ways to integrate natural ingredients in creating new treatment modalities.
These plant extracts seem to have a great degree of anti-microbial activity. Scientific data shows that of all the plants tested, an extract from a Taiwanese folk medicinal plant called Impatiens balsamina L. (Balsaminaceae) is the most efficient in treatment.
There is even a Chinese drug with patent and it contains two extracts from Chenopodium ambrosioides L. (CAL) and Adina pilulifera (AP) plants. It is a popular therapy among patients with gastritis and peptic ulcers in China. Phytomedicine is a great way to avoid unnecessary side-effects and toxicity unlike in other routine medications.
Vitamins
Recent studies show that people with HP infection have low vitamin C, D and E levels in their bodies. Once they test negative and get rid of the infection, these levels start to rise again. Therefore, scientists believe that vitamin supplementation can be useful in the process of HP eradication. Since these vitamins also act as antioxidants, they provide the added advantage of protection against gastric carcinoma, a serious but rare complication of HP infection.
Vaccination
Development of a vaccine is a great way to put an end to an infection with a vast global distribution. However, unfortunately, an effective vaccine is still not available up to date, despite all the efforts put into creating one. Although some projects are showing satisfactory results in animal models, without convincing evidence in clinical trials, they are not of much use either. Hopefully, scientists will soon come up with an effective solution to pull the plug for this problem.
Clinical practitioners are now leaning more towards susceptibility-guided therapy, which focuses on the emergence of antibiotic resistance. This allows them to avoid already misused antibiotics in the treatment process depending on the situation.
Most regions in the world have almost reached the point where antibiotic-based therapies can no longer be considered as the first line treatment option for HP infection mainly due to resistance. As a result, scientific communities in different parts of the world have gathered together to maintain databases, surveillance programs and share knowledge regarding resistant strains, and develop of new treatment modalities as a unit. They also monitor the effectiveness and safety of already existing methods of treatment.
We live in an era where the scientific knowledge regarding diseases is constantly changing. Surprisingly enough, even the simplest forms of disease-causing bacteria and viruses adapt and find new strategies to survive in response to whatever means we come up with to defeat them. These tiny pathogens are smart; but we human beings are smarter. (at least that’s how it’s supposed to be, right?) It is important that we stay ahead of the game all the time. As long as we keep coming up with new and efficient ways to beat these infections, we will have nothing to worry about.
References
- Ahmed, N., 2005. 23 years of the discovery of Helicobacter pylori: Is the debate over?
- O’Connor, A., Liou, J.M., Gisbert, J.P. and O’Morain, C., 2019. treatment of Helicobacter pylori Infection 2019. Helicobacter, 24, p.e12640.
- Hu, Y., Zhu, Y. and Lu, N.H., 2020. Recent progress in Helicobacter pylori treatment. Chinese Medical Journal, 133(3), p.335.
- Matsumoto, H., Shiotani, A. and Graham, D.Y., 2019. Current and future treatment of Helicobacter pylori infections. Helicobacter pylori in Human Diseases: Advances in Microbiology, Infectious Diseases and Public Health Volume 11, pp.211-225.