Table of Contents
Clinical Case Scenario-
A 40-year old female patient with chronic renal failure got admitted to the medical ward complaining of recurrent episodes of dizziness, syncope, and palpitations. Other than that, she also complained of mild nausea and difficulty in breathing. The patient is also on medications for depression for a long time.
On physical examination, the patient seemed to be in distress, slightly pale, and had an irregular pulse rate of about 200 beats per minute. We were also able to observe a slight drop in blood pressure.
Although the symptomatic presentation along with findings on physical examination would point towards a cardiac arrhythmia, we decided to wait until the results of the investigations arrived before making any hasty diagnosis.
In the end, all things considered, a final diagnosis of Torsades pointes with acute on chronic renal failure was made. But how could we arrive at such a diagnosis? What information led us to that conclusion. Let’s dissect into elements of this clinical case scenario to uncover everything.
Differential Diagnosis We Had in Mind
- Ventricular Tachycardia
- Ventricular Fibrillation
- Syncope
- Drug toxicity- antihistamines, antiarrhythmics
- Renal failure/dialysis-related complications
What is Torsades pointes?
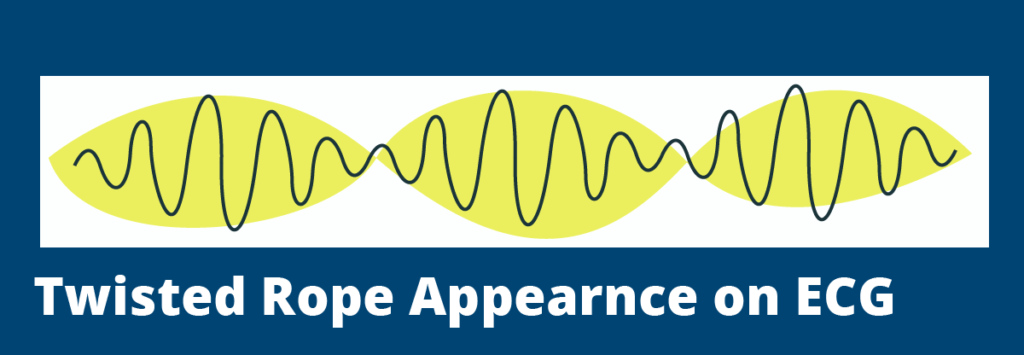
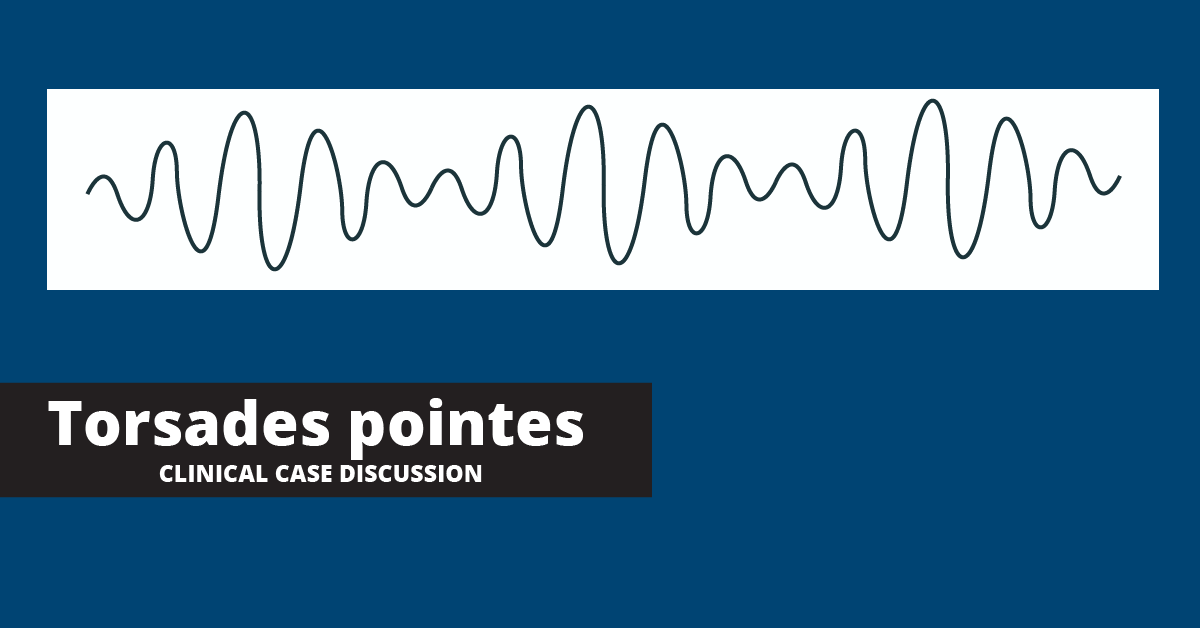
Torsades is a French term with the literal meaning of “twisting of the points”. This medical condition has gained this interesting name owing to its characteristic pattern on the ECG. Torsades pointes is a polymorphic or in other words, multi-shaped ventricular tachycardia that has a distinguishable appearance- as if oscillating around an axis.
The other significant feature that helps to detect this arrhythmia is the prolongation of the QT interval.
Torsades pointes is a very rare medical condition and is often transient. Data shows that females tend to exhibit this trait more than males on average.(1) If left untreated, torsades pointes have the potential of progressing into ventricular fibrillation. However, unlike ventricular fibrillation, torsades pointes often resolve spontaneously.
Pathophysiology
Torsades pointes occur as a result of the prolongation of the repolarization phase in the cardiac cycle. We all know that cardiac repolarization consists of three phases. In a normal person, during the third phase of repolarization, potassium ions are usually sent outside away from the cell membrane so that a more negative environment can be created inside the cell membrane. This phenomenon is known as the delayed rectifier potassium current as a positive current is formed outwards from the cell.
During torsades pointes condition, what happens is that this delayed rectifier potassium current is inhibited due to blocking of the potassium channels. As a result, the repolarization phase gets prolonged giving rise to a higher than normal QT interval. In such a background, when an ectopic beat is generated, it can result in the formation of the torsades de pointes pattern.
QT prolongation in torsades can be either congenital or acquired. However, in both conditions, blocking of potassium channels is the reason behind.
Congenital long QT syndrome
There are about 10 forms of congenital QT interval prolongation and all of them fall under three main categories as Type-1, Type-2, and Type-3. They occur due to genetic mutations and are autosomal dominant in inheritance.
Patients with prolonged QT intervals followed by torsades pointes are at more risk of developing syncopal attacks and sometimes even death as a result of ventricular fibrillation.
Acquired long QT syndrome
Acquired QT interval prolongation is mainly drug-induced. This occurs as a result of slowing down the metabolism of medications by the liver leading to increased blood concentrations. Drugs that can result in QT prolongation include;
- Class I-a, I-c, or III antiarrhythmic drugs
- Tricyclic antidepressants
- Phenothiazines
- Antivirals
- Antifungals
Sometimes co-morbidities like chronic kidney disease may also lead to QT prolongation. Patients with kidney disease often have deranged electrolyte and metabolic parameters in their bodies that can negatively affect the heart.
On the other hand, chronic kidney diseases may impair renal elimination of medications that could prolong the QT interval leading to unintended toxicity irrespective of dose adjustment according to the glomerular filtration rate (GFR).(2) This could have been the reason behind the torsades pointes of the patient in the clinical case we discussed, as she was also suffering from chronic renal impairment.
Other risk factors associated with prolonged QTc and Torsades include;
- older age > 65
- female gender
- hypokalemia
- hypocalcemia
- hypomagnesemia
- bradycardia
- heart disease
- diuretic use
Findings we looked for in the Clinical Examination
Quite similar to our patient, some individuals with torsades pointes may present with symptoms like syncope, dizziness, and palpitations. Some patients may develop clinical symptoms indicating hypoperfusion to the brain like reduced levels of consciousness.
However, about 50% of patients with the condition could be asymptomatic. In about 10% of patients, cardiac death could be the presenting symptom.
Here is a list of common physical signs that can be elicited in a patient with torsades pointes.
- Increased pulse rate (200 to 250 beats/minute)
- Low or normal blood pressure
- Pallor
- Diaphoresis
What Investigations Would Help Us Detect Torsades Pointes?
Investigations that we need to perform to detect torsades pointes are mainly two-fold. They include electrocardiography and basic laboratory investigations. The mainstay investigation is non-other than the electrocardiograph that would indicate any arrhythmias that might be going on.
Electrocardiograph (ECG)
There are very characteristic findings that would indicate the arrhythmia to be torsades pointes on an ECG. Some of them are listed below.
- Twisting of the QRS complexes around an isoelectric line (the polarity of complexes shifting around the baseline)
- Presence of complete 180° twist of QRS complexes in 10-12 beats
- QT prolongation of 0.60 s or longer
- QTc (corrected for heart rate) of 0.45 s or longer
- The ECG pattern may convert into a nonpolymorphic ventricular tachycardia or ventricular fibrillation spontaneously
Laboratory Investigations
Laboratory investigations would help rule out any underlying pathologies or metabolic derangements that may lead to the occurrence of cardiac arrhythmias like torsades.
- Basic electrolyte profile– May help detect electrolyte abnormalities like hypokalemia, hypomagnesemia, and hypocalcemia that may lead to QT prolongation
- Blood Glucose levels– Studies show that hypoglycemic patients are more prone to get QT prolongation and may further increase the risk of malignant arrhythmia in patients with long QT syndrome.(3)
- Cardiac enzymes– To rule out cardiac ischemia
- Cardiac Imaging– Chest X-ray and Echocardiographs to rule out structural heart disease in suggestive patients
- Other– Relevant investigations depending on etiological factors
How Can We Treat a Patient with Torsades Pointes?
The treatment for torsades pointes can be categorized into short-term and long-term management.
Acute Management
It is crucial to identify the risk factors and make timely interventions as necessary in the acute management phase. Let’s try to break down the steps that can be adopted in managing torsades acutely.
- The first step in the management should focus on establishing the hemodynamic stability of the patient.
- preventing the onset of torsades by identifying and targeting modifiable risk factors should be considered. This includes discontinuing any drugs that may further prolong the QT interval.
- It is also important to optimize the electrolyte profile of the patient. As one of the most important steps in acute management, correcting electrolyte abnormalities like hypokalemia, hypomagnesemia, and hypocalcemia to prevent the onset of torsades should be considered.
- Although most episodes of torsades pointes are self-limiting, some patients may progress into developing ventricular fibrillation. In patients who may develop hypotension or cardiac arrest from Torsades de Pointes, electrical cardioversion should be performed.
For a hemodynamically unstable patient in torsades who has a pulse, synchronized cardioversion (100J monophasic, 50J Biphasic) can be tried. On the other hand, the torsades patient who is pulseless should be defibrillated.
- As the first-line pharmacologic treatment for torsades, intravenous magnesium can be given. Magnesium is known for its ability to stabilize the cardiac membrane.
It is recommended to administer an initial dose of 2 g IV magnesium followed by an infusion of 1 gm to 4 gm/hr. The target is to keep the magnesium levels greater than 2 mmol/L. Once the magnesium level reaches 3 mmol/L or more, the infusion can be terminated.(1)
However, when the magnesium level reaches a value higher than 3.5 mmol/L, signs of magnesium toxicity may start to appear. They include respiratory depression, confusion, coma, and even cardiac arrest.
- When treating a patient with torsades, it is important to correct hypokalemia as well. Serum potassium levels below 3.0 mmol/l may cause significant Q-T interval prolongation and subsequently lead to torsade des pointes. Therefore, serum potassium levels should be maintained between 4.5 mmol/L and 5 mmol/L.
- For patients who do not respond well to magnesium therapy and continue to have intermittent episodes of torsades, using medications to increase the heart rate is available as an option.
Such medications that may increase heart rate include Isoproterenol, a non-selective beta-agonist, that increases the heart rate and shortens the QT interval.
Isoproterenol is administered IV with a dose of 10 mcg to 20mcg or an infusion titrated to maintain a heart rate of 100 bpm. However, in patients with congenital prolonged QT, using Isoproterenol is contraindicated as it can paradoxically lengthen the QT interval.
- The final option in the acute management of torsades pointes is to try override pacing. It is often used in the settings of frequent episodes of torsades or if torsade is refractory to magnesium therapy.
Temporary transvenous pacing of the atria is the common practice as it may help narrow the QRS complexes, giving rise to short QT intervals.
The target is to set a rate to overcome the patient’s intrinsic rate of ectopy. Ventricular rates of 90 bpm to 110 bpm are usually enough to overcome the arrhythmia. Some instances may require rates up to even 140 bpm.
Long-term Management
Since acquired long QT syndrome often resolves after treating the root cause, it often does not require any long-term therapy.
However, QT prolongation occurring due to congenital causes may require treatment in the long run. Often this includes treatment with Beta-adrenergic antagonists like Propranolol. But propranolol cannot be used in the acquired version of the long QT syndrome as the resultant bradycardia may itself precipitate torsades.
Permanent pacing, High left thoracic sympathectomy, and Implantable cardioverter-defibrillators (ICDs) are few other options that are available for the long-term treatment of torsades if beta-adrenergic therapy fails to provide satisfactory results.
Patient Counselling
Patient education is a highly important aspect of managing a patient with long QT syndrome or torsades. The patient should be advised regarding the risks of the disease and can be provided with emotional support or be directed to a patient support group.
It is important to make sure that the patient understands the risks of engaging in strenuous activities or competitive sports while having a disease condition like torsades because it can lead to grave outcomes like sudden cardiac death.
The healthcare provider should provide relevant education regarding measuring the pulse rate, and recognizing adverse effects of medications to the patients and caregivers alike. Furthermore, teaching and training family members how to provide basic life support is also of great importance.
What complications could arise in a patient with torsades pointes?
Although rare, the complications of this condition can be quite serious. The complications of torsades may vary from monomorphic ventricular tachycardia to ventricular fibrillation and sudden cardiac death.
What would be the prognosis of a patient with torsades pointes?
The prognosis of acquired long QT syndrome is quite good and often the condition may subside once the underlying cause is treated.
On the other hand, congenital long QT syndrome has a high mortality rate of 50% in 10-years in the absence of proper therapeutic interventions. With proper and timely treatment this may significantly reduce to about 3-4% over time.(4)
Conclusion
Although very rare, Torsade can easily become fatal if not diagnosed and treated at the right time. Patients often may present with a wide array of non-specific cardiac symptoms, but it is the ECG that is diagnostic. A patient management team that includes a physician, an electrophysiologist, a cardiologist, nurses, and a geneticist (if the patient has congenital long QT syndrome) is necessary for treating this condition. Advising not to engage in strenuous physical activities due to the risk of sudden cardiac death is paramount. At the end of the day, with close follow-up, accurate diagnosis, and timely intervention you will be able to save a patient with torsades pointes.
References
1. Cohagan B, Brandis D. Torsade de Pointes [Internet]. StatPearls. StatPearls Publishing; 2021 [cited 2021 May 8]. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29083738
2. Liu P, Wang L, Han D, Sun C, Xue X, Li G. Acquired long QT syndrome in chronic kidney disease patients [Internet]. Vol. 42, Renal Failure. Taylor and Francis Ltd; 2020 [cited 2021 May 8]. p. 54–65. Available from: /pmc/articles/PMC6968512/
3. https://www.ahajournals.org/doi/pdf/10.1161/CIRCULATIONAHA.116.024279
4. Torsade de Pointes: Overview, Pathophysiology, Etiology of Torsade [Internet]. [cited 2021 May 9]. Available from: https://emedicine.medscape.com/article/1950863-overview#a9