Sometimes patients walk in complaining about their jaws and teeth aching, but after examinations, they realize it’s not dental pain. Actually, it has nothing to do with dental care in the first place.
Trigeminal Neuralgia shows similar symptoms to dental pain or TMJ disorders (temporomandibular/jaw disorders) but as the name suggests, this condition is related to the nervous system in our body.
Trigeminal Neuralgia is described as the most excruciating stabbing pain a patient could experience in the face. A pain so sharp it stings and becomes unbearable, causing painful electrical sensations on one side of the face. Some may be short attacks, while others may last longer.
But what causes this unbearable pain? Could it lead to madness? Can it be cured? Read on to learn the A-Z’s of this curious disorder of the nervous system.
Table of Contents
Overview
Causes of Trigeminal Neuralgia
Trigeminal Neuralgia (sometimes known as tic douloureux) presents itself when the trigeminal nerve (one of the largest nerve series in the head) is blocked and disrupted.
There are two types of trigeminal neuralgia called Primary and Secondary.
Primary trigeminal neuralgia is associated with vascular compression of the nerve. The body is filled with a mix of nerves and blood vessels, intertwining and crossing each other to help the body function as it does and sometimes the blood vessel presses against the trigeminal nerve. Constant stimulation of this compression of the vessel against the nerve can wear out the protective insulation around the nerve (we call it the myelin sheath – myelin is a substance that wraps around nerves to help send faster signals to your brain). This exposes the nerve (and reduces the speed of stimulations). Nerves become sensitive and lead to extreme pain.
Because of the demyelination of the myelin sheath, trigeminal neuralgia may also cause other disorders including multiple sclerosis (demyelination of the myelin sheath) as well as dental conditions.
Secondary trigeminal neuralgia is usually known to be caused by pressure on the nerve by a different factor such as a tumour, a cyst, an injury to the face, or a medical condition that damages myelin sheaths. This means that conditions such as multiple sclerosis can be the cause of trigeminal neuralgia and can be caused BY trigeminal neuralgia as well.
The Trigeminal Nerve
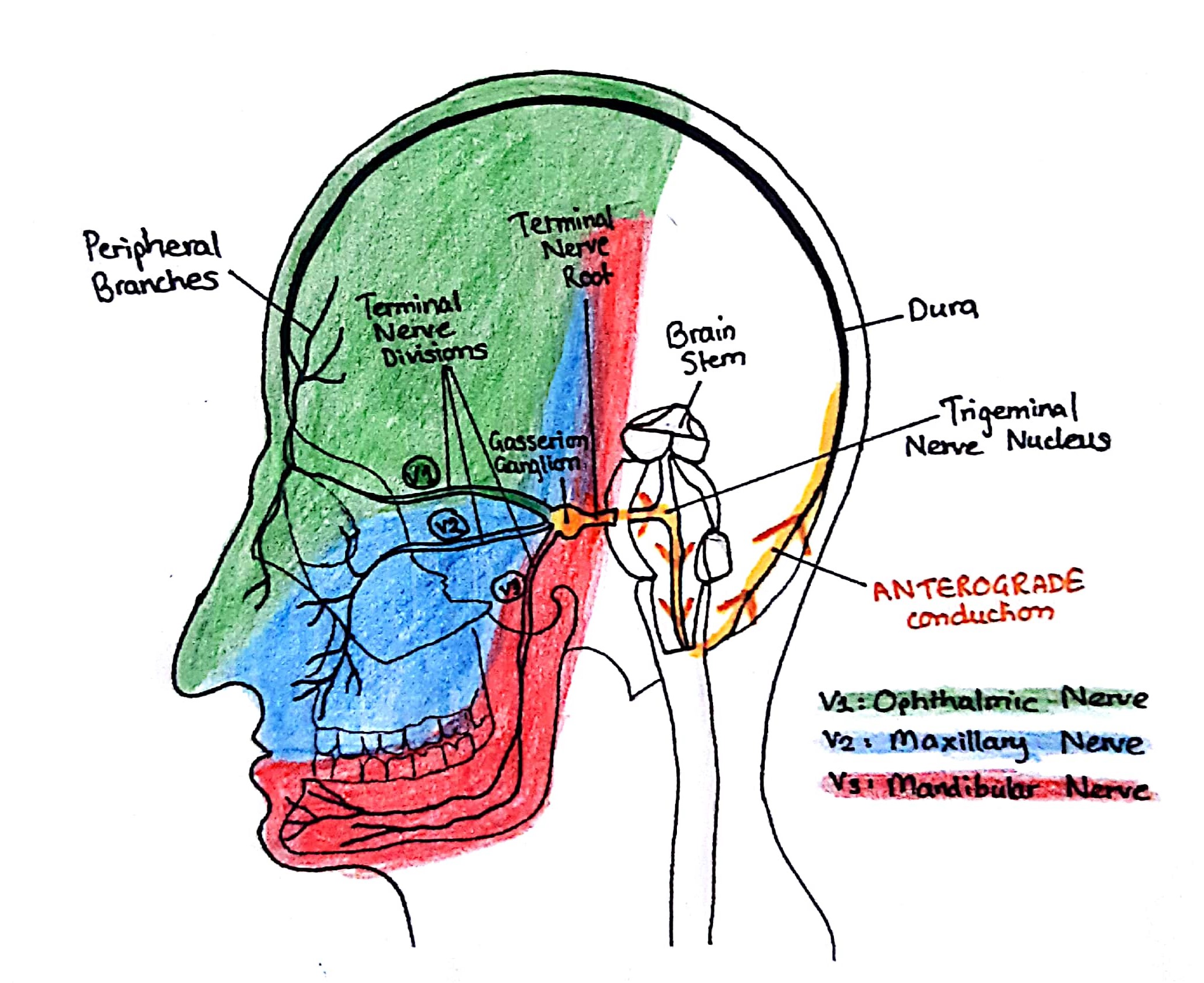
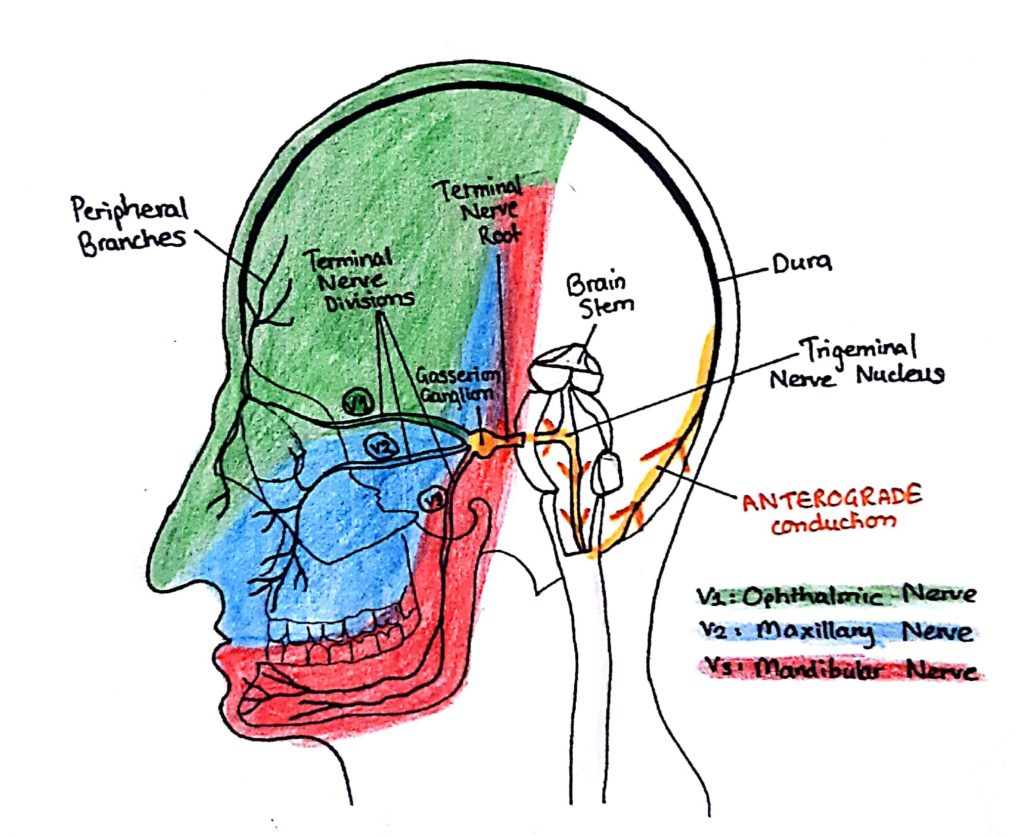
The Trigeminal Nerve is one of the larger sets of nerves in the head (cranial nerves) and is responsible for developing sensations on your face. It starts at the pons and spreads down the head and face. There are 3 nerves each of which has a special function.
- Ophthalmic Nerve (V1) – the first branch that controls sensation in your eyes, upper eyelid and forehead
- Maxillary Nerve (V2) – the second branch that controls sensation in your lower eyelid, cheeks, nostrils, upper lip and gum
- Mandibular Nerve (V3) – the third branch that controls the sensation of your jaw, lower lip and gum and muscles that are involved in chewing
Triggers
Every person is built different and so they will have different triggers. This condition is so sensitive and the smallest action such as touching your face or talking can act as a trigger for the pain.
Other triggers include;
- Shaving
- Eating or drinking
- Brushing your teeth
- Applying makeup
- Smiling or talking
- Washing your face
Symptoms
Most of the symptoms of trigeminal neuralgia are associated with pain in the face.
- Severe jabbing pain in the face that feels like an electric shock.
- Pain occurring with facial spasms
- Multiple attacks lasting days or weeks or even months
- Pain in the jaw, cheek, teeth, lips or gums
- Pain in one side of the face
- Attacks can become more frequent with time
Pain is usually first experienced in the upper or lower jaw, hence why many patients assume it’s a dental problem when the original root of the cause is neurological.
Pain can be classified as either Type 1 (TN1) or Type 2 (TN2). TN1 is classified as sharp and throbbing pain around your eyes, lips, nose, scalp and forehead. It can grow into more painful and more frequent attacks lasting longer and longer. TN2 pain is persistent burning pain however it may be less intense stabbing pain than TN1. However, the pain runs in cycles where the patient may feel frequent attacks of pain and then followed by weeks or months of little pain. The pain can also leave the patient with uncontrollable facial twitching hence the name “tic douloureux”.
Diagnosis
Trigeminal neuralgia may be hard to diagnose or commonly misdiagnosed as a different condition until much later when the original cause is determined. There are no specific diagnostic tests. In most cases, an MRI is done to check for tumors or MS that may affect the trigeminal nerve and if there is a blood vessel causing compression to the nerve, this can also be detected. Due to new medical advances, technology is being developed to determine the degree of compression on the nerve however, most of the time compression due to veins is not easily detected.
This is why patient background, history, symptoms and evaluation are important from the doctor and specialist.
Associated Disorders
Trigeminal Neuralgia Induced Migraines
Some patients with a history of migraine headaches may also experience headaches or pain in the head. Migraines are neurovascular disorders that cause a pulsating and recurring headache that may last from 4 hours to 4 days. They are usually accompanied by auras (a visual or sensory disturbance) alongside nausea, emesis (vomiting) or disturbed vision. And certain triggers including flickering lights, certain food (chocolate, eggs), or insufficient sleep may affect the onset of migraines.
Symptoms of migraines can be categorized into Autonomic, Cognitive and Sensory. Autonomic symptoms include those involuntary ones, beyond our control, such as vomiting, nasal congestion, yawning, frequent urination or even diarrhea. Cognitive symptoms include those affecting your psychiatry, including depression, irritability, or transient amnesia. And sensory symptoms are those related to the senses such as muscle tenderness, or cutaneous allodynia (an abnormal pain from non-harmful stimuli on normal skin).
Multiple Sclerosis (MS)
Scientists have found that trigeminal neuralgia could be an early symptom of MS because the body’s immune system attacks the myelin sheath wrapped around neurons. And when the myelin sheath is destroyed (demyelination) leading to symptoms like vision issues (blurred vision), muscle stiffness and spasms, or numbness along with many other symptoms.
And so the chances of you having MS increase your chance of developing trigeminal neuralgia. Both MS and trigeminal neuralgia occur more often in women than men.
For treatment for this population of patients, surgery is possible however it is less predictable and long-lasting in patients with MS with a greater risk of complications during craniotomies.
Temporomandibular joint syndrome (TMJ)
TMJ is a jaw condition where the muscle controlling jaw movement malfunctions and causes great pain in your jaw joints and facial pain hence why it’s often confused with trigeminal neuralgia as TMJ disorders exhibit similar facial pains.
To differentiate from trigeminal neuralgia, symptoms of TMJ disorders include; neck pain near your ear, jaw locking, difficulty chewing food, frequent headaches or jaw muscle spasms which are uncommon with trigeminal neuralgia.
Treatment
Non-surgical
Non-surgical treatment options are available to help alleviate the pain. First-line drugs for primary and idiopathic trigeminal neuralgia are pharmacologic therapy.
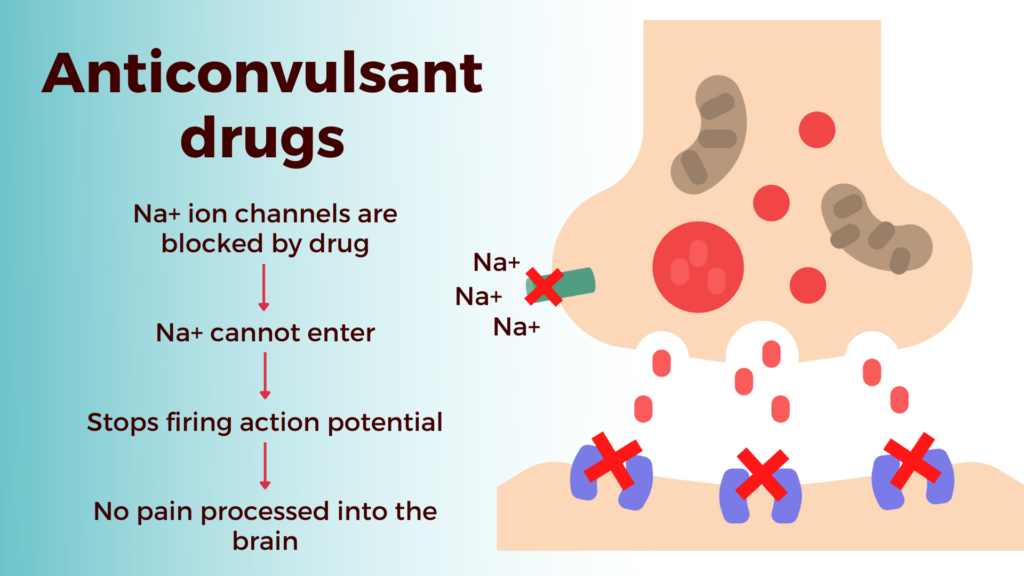
- Anticonvulsant drugs (Carbamazepine, Gabapentin)
This drug usually starts in lower doses and then your doctor would increase the dosage gradually until the medication controls the pain. This is effective in the earlier stages of the disease. But for some patients, the sensitivity to this drug reduces over time bearing no effect on the pain. The mechanism of action for anticonvulsant drugs (also known as antiepileptic drugs) is commonly through the modulation of voltage-gated sodium channels. These drugs act to bind and block the sodium channels, reducing the firing of action potentials and reducing pain.
Side effects: dizziness, drowsiness, confusion, nausea, memory problems, sleepiness, double vision
- Antispasmodic drugs (Baclofen)
Drugs such as Baclofen are known to be muscle relaxants however they can also be used to treat trigeminal neuralgia. They activate inhibitory actions. Therefore, they reduce the excitatory stimulation of action potentials and reduce pain in patients.
Side effects: confusion, drowsiness, nausea, dry mouth, problems sleeping, blurred vision
There are many other drugs and medications used for different patients as each patient has their own response to the drugs and drug effects on the body.
Surgical treatment
There are two types of surgical treatment for trigeminal neuralgia, open surgery and lesioning procedures.
Open surgery is called Microvascular Decompression, a surgery that is advantageous for patients with vascular compression acting on the nerve. In this procedure, the surgeon moves the blood vessel away from the area of compression and frees the nerve so that the nerve can recover and function normally without causing pain. While this type of surgery is effective, it is also open surgery which means a craniotomy is done to open the skull and some certain risks and complications come with this, including facial weakness or numbness, decreased hearing, or even strokes. However, for most patients, this procedure ensures that they can live a pain-free life for over 10 years showing to be one of the most effective long-term treatments for trigeminal neuralgia.
Diagram 4.0: Neurosurgery done my expert neurosurgeons using advanced equipment and machinery to help guide them through intricate surgeries such as Microvascular Decompression
Lesioning procedures are interventions that help prevent the nerve from causing pain to the face. These can be divided into percutaneous procedures:
- Glycerol injections
- Radiofrequency lesioning
- Balloon compression
Percutaneous glycerol rhizotomy basically uses a needle to inject glycerol into the space where the nerve divides into three aiming to damage the nerve and stop the transmission of pain signals to the brain. This helps lessen the pain processed and felt by the patient. While this procedure relieves pain, some patients have a later recurrence of pain.
Percutaneous radiofrequency rhizotomy helps treat trigeminal neuralgia through heat (electrocoagulation). Heat is passed through electrodes (a needle is inserted through the cheek) destroying the nerve that causes pain and stops the pain signal from reaching the brain. Some patients experience temporary facial numbness.
Percutaneous balloon compression uses a needle passed through the cheek to access the trigeminal nerve and a balloon is passed through to the nerve through a catheter. The balloon is inflated at the location the fibres produce pain and so the balloon compresses the nerve, destroying the nerve fibres.
We’ve talked about non-surgical pharmaceutical treatment and surgical treatment but what about natural treatment? What can we do at home to ease the pain? Some have suggested acupuncture (a Chinese traditional medication using thin needles) or aromatherapy (using plant oils to assist in healing), meditation or yoga. While these may do very little to help, the psychological impact of trigeminal neuralgia is also important to consider because those with this condition also have a higher risk of developing psychiatric disorders including depression, anxiety, or sleep disorders. And when you think about it, it makes sense. Wouldn’t you reach a point of frustration and depression if your face ached every time you moved? This is why simple things like aromatherapy may be helpful to ease the mind. While drugs and surgical solutions do their best to cure the pain, it is important to note mental health is just as important. Your mental health could be affected through the disorder or through drugs and medication itself and it’s always best to be aware and careful as doctors nurse you back to good health.
Conclusion
Trigeminal neuralgia is a strange and painful condition showing signs of electric stabbing pain in your face primarily due to vascular compression of the trigeminal nerve in the deep structures of the brain. While the symptoms of the disorder are painful, these symptoms can be commonly mixed with dental disorders or other neurological conditions. However, through accurate diagnosis, treatment is available through therapeutic drugs or surgical solutions. Microvascular Decompression is the most common and long-lasting surgical treatment option preferred by many doctors and patients alike and through treatment; patients can lead a healthier pain-free lifestyle.
References:
Yadav et al., (2017), ‘Trigeminal Neuralgia’, Asian Journal of Neurosurgery, 12(4), 585-597
Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5652082/
Gambeta, Chichorro and Zamponi (2020), ‘Trigeminal neuralgia: An overview from pathophysiology to pharmacological treatments’
Available at: https://doi.org/10.1177/1744806920901890
Huff and Daly, (2021), ‘Neuroanatomy, Cranial Nerve 5 (Trigeminal)
Available at: https://www.ncbi.nlm.nih.gov/books/NBK482283/
Bennetto et al., (2007), ‘Trigeminal neuralgia and its management’, BMJ, 334 (7586), 201-5
Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1782012/
Wu et al., (2015), ‘Risk of psychiatric disorders following trigeminal neuralgia: a nationwide population-based retrospective cohort study’, The Journal of Headache and Pain
Available at: https://thejournalofheadacheandpain.biomedcentral.com/articles/10.1186/s10194-015-0548-y