Table of Contents
Overview
With Halloween just left behind, there’s plenty of spookiness to behold, in the form of mummies, zombies, and various other characters which do not belong in the plane of the living. Of course, this is all thanks to flawless costumes and talented application of makeup. It’s all just fun and games lasting a single night of the year.
Nothing to truly worry about.
It’s not like walking corpses truly exist. They don’t, do they?
…What if they do?
What if some walk among us as the dead yet undead?
Sounds fantastical? Perhaps. But is there some truth to it?
Eerily, yes, there is. Because there have been people among the world’s population who have existed as walking corpses. And it certainly lasted for more than a single night a year.
Case Report:
The most famous case of such a bizarre account of a person is undoubtedly that of Mademoiselle X, documented and described by the French neurologist, Dr. Jules Cotard.
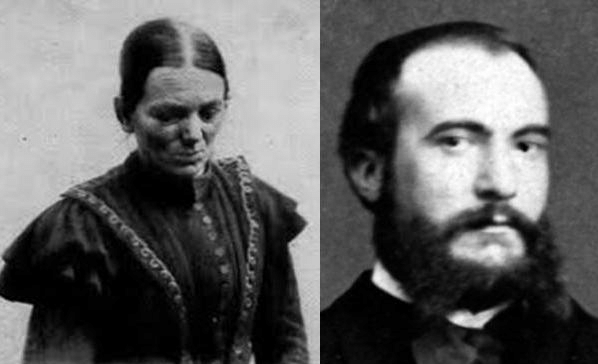
Dr. Jules Cotard (1840–1889) was not only a Parisian neurologist and psychiatrist but was also a former military surgeon. He was a leading expert on cerebral atrophy (degradation of the brain) at the time thanks to his various ventures into experimental induction of brain atrophy via embolization in animals as well as his studies in the pathological aspects of cerebral atrophy.
In 1882, he encountered a female patient (whom he thereafter referred to as Mademoiselle X to protect the patient’s rightful privacy) in a Parisian hospital.
She was 43 years of age and had a quite usual set of complaints.
According to this patient, she had “no brain, no nerves, no chest, no stomach, no bowels – there was nothing left of her but the skin and bones.” She also made claims related to religious and spiritual beliefs, denying the existence of God and the devil, and also stating that she no longer had a soul, and was only “a disorganized body”. She declared herself immortal, in the sense that due to her lack of normal human physical and spiritual parts, she would be unable to die a natural death. She said that she would “live forever unless she was burned, fire being her only possible end”.
As it turned though, there was no need for a Viking–style funeral pyre; since she stopped eating, her foregone conclusion that she was missing her internal organs made her dead certain that she no longer needed any form of sustenance. Ultimately, this patient died of starvation.
About Walking Corpse Syndrome
This strange mentality of believing themselves to be deceased can be observed in patients suffering from a rare neuropsychiatric disorder known as Walking Corpse Syndrome.

It is also known as Cotard’s Syndrome or Cotard’s Delusion, named after Dr. Jules Cotard who first presented his diagnosed case to the world at a lecture he delivered at the Société Médico-Psychologique in Paris held on 28th June 1880.
Cotard’s Syndrome patients labor under the delusion that they are dead, non-existent, putrefying, or have lost their internal organs or their blood.
For example, there has even been another documented case of a female patient who complained that she was dead and smelled of rotten fish.
Cotard described this disorder as ‘le délire des négation’ which translates into: the delirium of negation.
Clinical Presentation (Symptoms & Signs)
Walking Corpse Syndrome is characterized by its main symptom – the delusion of negation. Patients believe they are missing parts of their bodies, that they are dead, or even that they do not exist at all.
Other signs and symptoms of Walking Corpse Syndrome include:
- Decreased socialness – they may altogether stop speaking and communicating with those around them
- Loss of interest
- Loss of appetite
- Lack of concentration
- Hopelessness and depressive emotions
- Anxiety – can be taken as an early symptom
- Feelings of guilt – this is one of the less common symptoms
- Auditory hallucinations – in the form of voices that convince them that they truly are either dying or already dead
- Ceasing to eat – they stop eating since they are sure they are no longer alive and therefore do not require food or any other form of nourishment
- Lack of sensitivity to pain
- Insomnia
Etiology
Researchers have different theories as to what causes Cotard’s Syndrome, how, and why, but none of these have been proven.
Cotard’s Syndrome has even been hypothesized to have a genetic factor. However, there is no evidence to confirm this.
Although the cause is uncertain, this disorder is believed to be a manifestation of a graver condition in which the brain is affected, such as:
- Dementia
- Encephalopathy
- Epilepsy
- Migraine
- Multiple Sclerosis
- Parkinson’s disease
- Cerebrovascular accident (CVA)
- Subdural Hemorrhage (SDH)
- Trauma (leading to damage in relevant areas of the brain)
Another possible cause of Cotard’s Delusion is medication.
Drugs such as Acyclovir and Valaciclovir (prodrug of Acyclovir) contain CMMG [Carboxymethoxymethylguanine] – which may result in patients having adverse reactions following metabolization of these drugs.
Epidemiology
Walking Corpse Syndrome is very rare – as of early 2022, there were just 200 diagnosed cases globally.
While it is possible to develop this disorder at any age, people of age 55 and above make up most of the recorded cases. But a small number of patients of younger ages have also been noted in the past.
Among the documented cases, females seem to be predominantly affected.
Associated Conditions
Walking Corpse Syndrome has been associated with neurological conditions such as:
- Cerebral atrophy
- Malformation of cerebral arteries and veins
- Cerebral infarction
- Superior sagittal sinus thrombosis
- Brain tumors; especially of the parietal lobe
- Temporal lobe epilepsy
- Catatonia
Other associated conditions include:
- Syphilis
- Typhoid fever
- Severe mental retardation
- Injury to the limbic system
Mental disorders which may increase the risk of a patient developing Walking Corpse Syndrome:
- Bipolar disorder
- Dementia
- Capgras Syndrome
- Post-partum depression
- Depersonalization disorder
- Dissociative disorder
- Psychotic depression
- Schizophrenia
- Substance abuse
Pathophysiology
Cotard’s Syndrome has been hypothesized to be due to lesions occurring in the parietal lobe in the cerebrum of the brain.
It may also be caused by the misfiring of neurons found in the fusiform gyrus as well as the amygdalae.
FUSIFORM GYRUS:

Location: lies on the basal surface of the temporal and occipital lobes
Function: helps in recognizing perceived faces, and reading
AMYGDALAE:
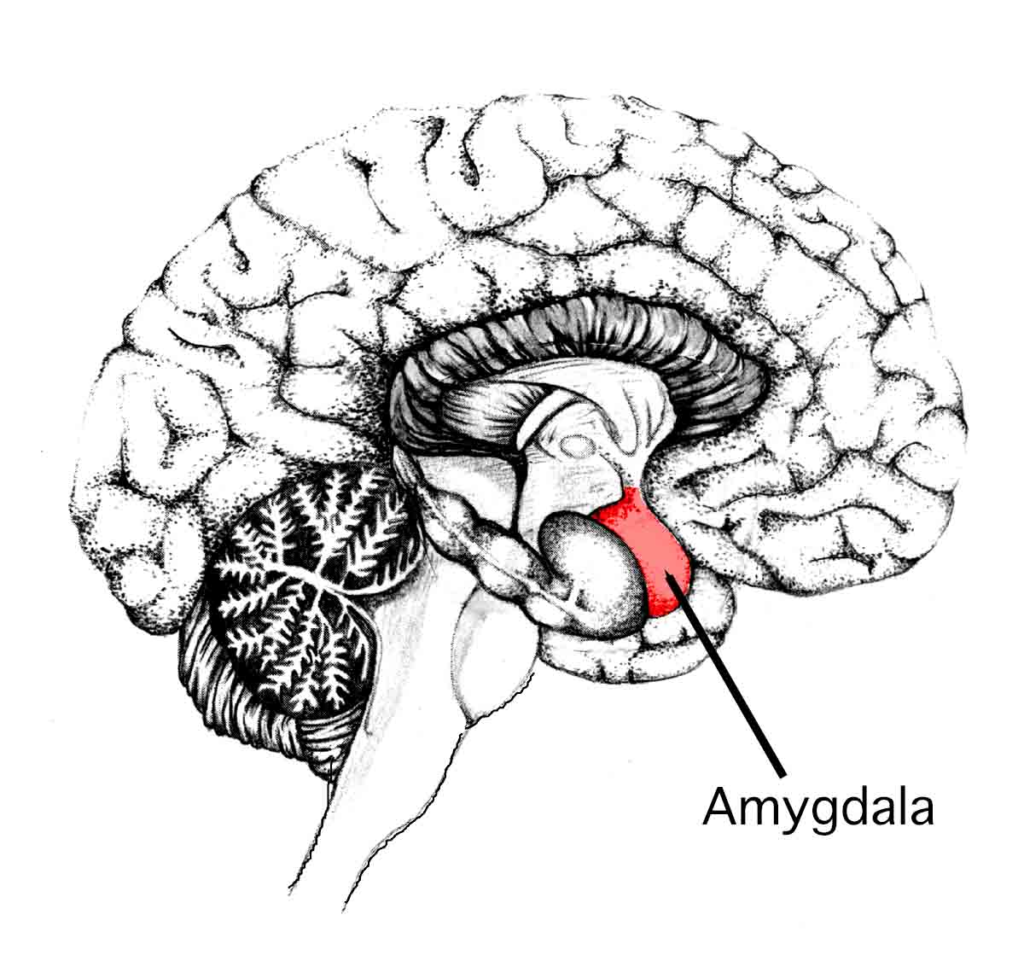
Location: located deep within the temporal lobes of the cerebrum
Function: processes the emotion of fear, and theoretically plays a role in facial perception
Therefore, dysfunction of these two areas which are necessary for facial identification and recognition, and reaction, leads to disconnection. Any face seen by the patient may not be recognized. This, chillingly, means that the patient may not only be unable to recognize others but also that they may no longer recognize themselves upon perceiving their face.
Bizarrely, when looking into their reflection, no sense of familiarity is elicited. Instead, they may feel as if they are simply gazing into the face of a stranger. This disconnection, known as derealization, may eventually end up with the patient concluding that they are no longer alive.
Of course, this is just one of the multitude of ways that a person may develop Cotard’s Syndrome, and due to the lack of solid theories, it is difficult to pinpoint just what may cause a patient to come to see themselves as the living dead.
Stages of Walking Corpse Syndrome
Walking Corpse Syndrome can be divided into three stages:
- Germination stage – This is when the initial symptoms appear, such as features of:
- depression
- cenesthopathy (feeling abnormal sensations within the body)
- hypochondria (an unnecessary worry or fear that one may have developed a grave illness when in fact they are quite healthy)
- Blooming stage – The syndrome fully develops, with obvious manifestations, especially with the patient alluding to the characteristic delusion of negation.
- Chronic stage – Disease continues to severely affect the patient
A cohort study of 100 diagnosed patients revealed:
- 45% displayed denial of life
- 55% had delusions of immortality (in the context of being unable to naturally die in their state of being)
Progression of Walking Corpse Syndrome
According to Dr. Cotard, patients suffering from this disorder can present with various degrees of severity.
In less severe cases – patients are plagued by feelings of despair and self-hate, akin to depressive disorders

In more severe cases – patients have accepted delusions that they no longer belong in the world of the living. This may be accompanied by chronic depression.
Patients of Cotard’s Syndrome who have developed strong delusional beliefs of their state of non-existence will not pay attention to their basic needs anymore.
While withdrawing from society and their loved ones, they will furthermore disregard their physical health, personal hygiene, and even fundamental requirements such as food and water.
Walking Corpse Syndrome in progressive stages affects the patient so much they can no longer make sense of their reality and are rendered unable to distinguish fact from fiction. Perhaps, for this reason, patients with Cotard’s Syndrome are sometimes compared to patients suffering from schizophrenia, but the majority of the recorded cases of Cotard’s Syndrome do not include visual or auditory hallucinations.
What is alarming is that these patients in later stages attempt self-harm and suicide.
The suicidal attempts are thought to be because patients may find that those around them, possibly including their health professionals display skepticism of their words. For instance, a patient with Cotard’s delusion may point out to others that he/she is dead or non-existent but may be met with incredulity or simply brushed off. Such patients may try to prove their condition – as perceived by their altered sense of reality – and attempt to commit suicide to show that since they are already dead, they are unable to die a second time.
Some patients may attempt suicide because they feel that the body they are inhabiting and the surroundings they are living in are strange and unfamiliar to such a degree that this unfamiliarity causes them to become distressed and lose touch with reality. Patients who struggle in this way might attempt to end their life to escape that upsetting existence.
Investigations for Walking Corpse Syndrome
There are a few ways of confirming this disorder via investigations.
Neuroimaging can help discover lesions in the brain causing Cotard’s delusions. These include:
- CT – Computed Tomography scan
- MRI – Magnetic Resonance Imaging
- PET – Positron Emission Tomography
Changes in the brain seen via neuroimaging in patients with Cotard’s Syndrome include:
- Changes in the frontal lobe
- Generalized loss of brain volume
- Bilateral / Right-sided hemispherical lesions
- Ischemic changes in the brain mass
Electroencephalogram (EEG) may show some non-specific slowing.
Diagnosis of Cotard’s Syndrome
Walking Corpse Syndrome can be considered to be a symptom of an underlying disease, rather than a disorder in and of itself.
Since much of the information currently available on Cotard’s Syndrome is still under a degree of doubt, medical practitioners who encounter patients with features suggestive of Cotard’s Delusion have a hard time diagnosing the condition. Without hard and fast guidelines to standardize and support the diagnosis of Walking Corpse Syndrome, doctors often resort to using the safer approach of first ruling out all other conditions similar to Cotard’s Syndrome (differential diagnosis) which can also be what the patient is having.
Walking Corpse Syndrome has not been included in the DSM (Diagnostic and Statistical Manual of Mental Disorders) as of yet.
Due to these problems, patients may go undiagnosed by healthcare personnel.

Management
After a successful diagnosis of Walking Corpse Syndrome, the patient must be assessed for immediate concerns. For instance:
Is the patient liable to attempt self-harm or suicide? – if there is any suspicion at all, precautions must be taken to prevent this
Is the patient a danger to himself or others? – if the patient displays signs of agitation or aggression measures must be taken to ensure the safety of all those involved
Is the patient’s life at risk due to poor physical health? – Late presentation may include starvation or dehydration; if so these should be corrected first using IV fluids
Once the immediate problems have been identified and managed, the treatment plan for the patient can be decided.
Treatment Options
Amongst the few methods of treating Walking Corpse Syndrome is the approach of first identifying and treating the causative problem.
Fortunately, although this disorder may be problematic to encounter, there are several treatment options.
- Pharmacotherapy – a combination of drugs is required for effective treatment
- Mood stabilizers
- Antipsychotics
- Antidepressants
- Antianxiety drugs
- Electroconvulsive Therapy (ECT) – this can be administered to help with depressive symptoms seen in most Cotard’s Syndrome patients.
- Psychotherapy – commonly known as ‘talk therapy
- Cognitive Behavioral Therapy (CBT) – is helpful in processing a patient’s thoughts, emotions, and behaviors and how they correlate to each other.
Other treatment options which may be necessary depending on the state of the patient include:
- Rehydration – if features of dehydration are present, especially in the later stages of the disease
- Cessation of administration of inducing drugs – if any
- Careful administration of sedatives – only if the patient is prone to violence incurred by the delusion of the disease
Electroconvulsive Therapy (ECT)
In past documented cases, a combination of pharmacotherapy and electroconvulsive therapy (ECT) has been successful in gradually bringing the patients out of their nihilistic delusions. However, electroconvulsive therapy does carry its risks:
- Nausea
- Confusion
- Memory loss
- Myalgia (muscle pain)
Nevertheless, since the pros outweigh the cons, ECT is still one of the main treatments for bringing the patient out of their depressive state of believing themselves to be walking corpses.
Who are at risk of developing Walking Corpse Syndrome?
There are patients, especially in the neuropsychiatric sector of disorders who are predisposed to develop Walking Corpse Syndrome.
Many noted cases are of patients who had a previous history of mental disorders.
For example:
- Anxiety
- Depression
- Schizophrenia
- Substance misuse
- Bipolar disorders
Others had suffered brain damage which lead to Cotard’s Syndrome. The brain damage could be visualized on radiological investigations such as CT and MRI scans.
The brain damage specifically could be, as previously discussed, a result of lesions such as:
- CVA (Cerebrovascular Accident)
- Trauma
- Thrombosis (Blood clot)
- Brain tumor
Complications of Cotard’s Syndrome
Many of the complications of Walking Corpse Syndrome arise when the disorder has gone undiagnosed for some time and the patient deteriorates further mentally, and as a consequence, physically.
Complications:
- Starvation – leading to extreme physical weakness and severe loss of weight, even emaciation
- Dehydration – leading to declining in awareness, and later even risk of kidney failure
- Nutritional deficiencies – malnutrition; with long-term loss of appetite
- Suicidal attempts – may be preceded by attempts to harm themselves

Prognosis
Patients having Walking Corpse Syndrome do not have to live their entire lives believing they are already dead. Patients who are diagnosed get better with treatment which usually includes drugs and electroconvulsive therapy, among others.
Almost all patients who receive proper treatment show obvious improvement, starting with the discarding of their delusion of negation, then slowly accepting they are indeed still alive, and beginning to take care of themselves again with proper nourishment and returning to their standard of personal hygiene. With time and continued medical attention, they reform connections with their friends and family and slowly integrate themselves back into society.
With successful treatment, patients who once believed they were dead and gone and nothing but corpses will reclaim their lives.
DID YOU KNOW?
Despite the lack of mention of Walking Corpse Syndrome in standard databases of mental disorders (notably the DSM), there have been cases and articles published about Cotard’s Syndrome.
- Betwixt Life and Death: Case Studies of the Cotard Delusion (1996)
- Recurrent Postictal Depression with Cotard Delusion (2005)
There are other publications, written by various psychiatrists, neurologists, researchers, and others, all of whose curiosity had been roused by this peculiar phenomenon of people among us claiming to be the dead among the living. While it may be enough to chill the blood of the living, it is also fantastical enough to drive a strong academic interest.
Another famous case of suspected Walking Corpse Syndrome is Per Ohlin, a musician famous in the genre of black metal music.
Per Ohlin of Mayhem
Per Yngve “Pelle” Ohlin (1986-1991) was a Swedish musician who is best known as the lead vocalist and songwriter for the black metal band Mayhem. What was unique about Per Ohlin who went by his stage name “Dead” was his unparalleled fascination with death and everything to do with dark mysticism. At only 22 years of age, he committed suicide, after a life of jarring musical performances, where he used everything in his arsenal to embody death including the use of ‘corpse paint’ and funeral pamphlets, and his passion for the darker arts.
He had positioned himself in the woods – in which he claimed to feel at peace as they removed him from the modern world – and slit his throat and wrists and also shot himself in the head with a bandmate’s shotgun.
The tragic and perplexing suicide note he left behind contained some alarming statements: “…It was the intention that I would die in the woods so that it would take a few days before I was possibly found. I belong in the woods and have always done so. No one will understand the reason for this anyway…”
Sometime after his mysterious suicide, Per Ohlin was not only hailed as a true devotee to the subgenre of black metal thanks to his unprecedented and even disturbing acts on stage but was also speculated to have struggled with a case of undiagnosed Walking Corpse Syndrome. It is equally likely that his fascination with the afterlife stemmed from the dreadful near-death experience he had resulting from a splenic rupture with massive internal bleeding, following a horrific bullying incident when he was a ten-year-old schoolboy.
While it has never been confirmed that he suffered from Cotard’s Syndrome, his name has been mentioned in possible unrecorded cases of this disorder.
Summary
Patients of Walking Corpse Syndrome have strong delusions of negation
Walking Corpse Syndrome, also known as Cotard’s Syndrome or Cotard’s Delusion, is a rare neuropsychiatric disorder of unconfirmed etiology. These patients struggle with nihilistic delusions leading them to believe that they are already dead or missing their organs or their blood. First described in 1880 by Parisian neurologist Dr. Jules Cotard, this disease has yet to be included in standard databases of mental illnesses, which consequently means that diagnosis of the condition is challenging. Although highly unusual and in some cases difficult to deal with, patients with Cotard’s Syndrome have a good prognosis with proper treatment – especially psychiatric drugs and electroconvulsive therapy (ECT).
Therefore, those patients who think of themselves as void of life and belonging in the afterlife can be gradually made to see that they still have a whole life ahead of them to lead, and thus, the walking corpses are no longer corpses, but alive.
These “dead” will live again.
Cotard’s Syndrome patients are not beyond help
REFERENCES:
WebMD:
https://www.webmd.com/schizophrenia/cotards-syndrome
Wikipedia:
https://en.wikipedia.org/wiki/Cotard_delusion
PMC:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4271387/
Psychiatry Online:
https://neuro.psychiatryonline.org/doi/10.1176/appi.neuropsych.17010018
Neurology:
https://n.neurology.org/content/58/9/1400
Gizmodo:
https://gizmodo.com/how-to-psychologically-treat-a-walking-corpse-1495363120
Medium:
https://medium.com/lessons-from-history/mademoiselle-x-living-while-dead-8fe06146b711
Metal Injection:
IMAGE REFERENCES
Walking Corpse Syndrome also known as Cotard’s Syndrome
Dr. Jules Cotard – French neurologist
https://en.wikipedia.org/wiki/Cotard_delusion
Mademoiselle X – the famous case of Walking Corpse Syndrome described by Dr. Cotard in 1880
Walking Corpse Syndrome; alluding to the patient’s belief they are nothing more than the living dead
https://youmemindbody.com/mental-health/Cotard-Delusion-The-Worlds-Most-Terrifying-Mental-Illness
Mid-sagittal view of the brain, showing the right hemisphere: Fusiform gyrus basal to temporal & occipital lobes
Exterior view of brain – Amygdala located deep within the cerebrum of brain
Depressive states are commonly seen in Cotard’s Syndrome patients
Cotard’s Syndrome patients can struggle with their own reality
https://www.self.com/health-conditions/depression
Electroconvulsive Therapy (ECT)
https://www.medpagetoday.com/psychiatry/bipolardisorder/99401
Emaciation is a result of patients forgoing their physical health and nourishment because of their nihilistic delusions
https://www.shutterstock.com/image-photo/girl-anorexia-turned-back-spine-ribs-1526605958
Per Ohlin of Mayhem
https://www.pinterest.com/pin/537406168033112953/
Patients of Walking Corpse Syndrome have strong delusions of negation
https://ceotudent.com/en/those-who-believe-they-are-dead-walking-corpse-syndrome
Cotard’s Syndrome patients are not beyond help
