Appendicitis is a common surgical case which you find in your everyday clinical practice. This chapter covers everything you need to know about Appendicitis.
Table of Contents
Let’s begin with a Clinical scenario:
Mr. X, a 24 year old male presented with 1 day history of Periumbilical pain which shifted to right Iliac fossa over few hours. He complains of constant pain which worsens on coughing or moving around. He is also having Fever, nausea, vomited few times over last 24 hours, and reduced appetite. He is a otherwise healthy person.
Clinical examination was as follows. General examination revealed he was feverish with flushed skin, slightly tachycardic, tachypnoeic. Abdominal examination revealed tenderness, guarding in right lower quadrant. When palpating in the left lower quadrant, he reports pain in the right lower quadrant. Active flexion of his right hip and internal rotation of the right leg reproduces his pain.
Laboratory investigations showed Neutrophil leukocytosis, elevated CRP. USS abdomen showed inflamed appendix with some free fluid.
The diagnosis of a Perforated Appendix with evidence of peritonitis is made.
Before moving on to the case of a perforated appendix, let’s first look at acute appendicitis.
What is Acute appendicitis?
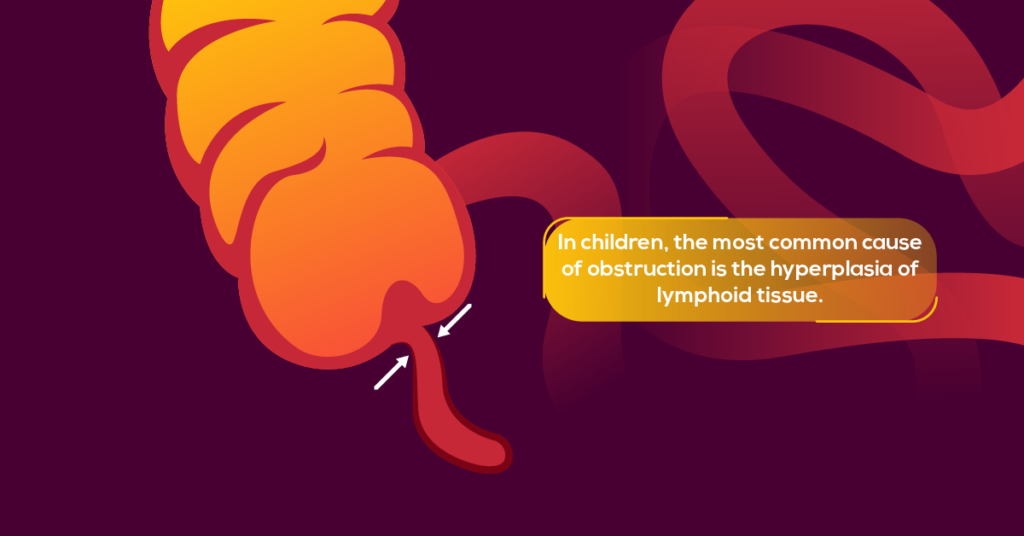
It is the acute inflammation of Appendix due to the obstruction of the lumen. The commonest causes of obstruction are by a feacolith( hard lump of obstructing faeces) or hyperplasia of lymphoid tissue.
Also, foreign bodies, Malignancy( carcinoid and adenocarcinoma), Parasitic or fungal infections, Inflammatory bowel disease and Trauma are recognized causes.
Fun fact: Latest research has shown appendicitis can occur in the presence of a patent lumen as well.
How it causes perforation?

Due to the obstruction of the lumen appendix get distended, causes bacterial overgrowth. With that, intraluminal pressure builds up and causes venous and lymphatic congestion, ulceration and transluminal spread of infections through the wall. This inflammation results in impaired blood flow, ischemia, necrosis and eventually Perforation.
Perforated Appendix can cause generalized peritonitis or sometimes the defect seal itself off against adjacent structure like omentum forming a mass. It is called an Appendicular mass or abscess.
Differential diagnosis for acute appendicitis presentation
General.
- Right side ureteric stones
- Pyelonephritis
- IBD/ terminal ileitis
- Gastroenteritis
- Gall stones
- Perforated duodenal ulcer
- Diverticulitis
- Ischemic colitis
Males.
- Testicular torsion
- Epididymo orchitis
Females.
- Ectopic pregnancy
- Pelvic inflammatory disease
- Ruptured/torted ovarian cyst
- Endometriosis
- Mittelschmerz pain
Children.
- Mesenteric adenitis
- Meckel’s diverticulum
- Intusucception
- Henoch- Schonlein purpura
- Following are some of the differentials and their clinical symptoms and signs which helps to distinguish from appendicitis,
| Clinical features | |
| Right side ureteric stones | Colicky abdominal pain, loin to groin pain, dysuria, hematuria, Nausea, Vomiting |
| Pyelonephritis | Fever, dysuria ,hematuria, renal angle tenderness |
| Cholecystitis/ Gall stones | Right upper quadrant pain radiating to back, pain worsen with fatty meals, nausea, vomiting, fever |
| Inflammatory bowel disease | Abdominal pain, blood and mucous diarrhoea, weight loss, Anemia, enterocutaneous fistula/ fissures |
| Gastroenteritis | Abdominal pain, nausea, vomiting, watery diarrhoea or bloody diarrhoea (dysentery) |
| Perforated duodenal ulcer | Acute onset epigastric pain, rigid abdomen, dyspepsia, history of peptic ulcers/ NSAIDs use |
| Mittelschmerz | Mid cycle pain ( physiological) |
| Ischemic colitis | Abdominal pain after having a meal, nausea, vomiting, history of peripheral vascular disease/ smoking |
| Testicular torsion | Sudden onset excruciating pain in scrotum, high lying testis, tender hemiscrotum |
| Epidydimo-orchitis | subacute pain, fever, dysuria , tender scrotum, history of sexual promiscuity in some cases |
| Ruptured Ectopic pregnancy | Abdominal pain, vaginal bleeding, period of amenorrhea, anemia( rarely hemorrhagic shock) |
| PID | Purulent vaginal discharge, dysuria, fever, cervical motion tenderness , gonococcal or chlamydia infection |
| Ovarian torsion | Sudden onset pain, adnexal mass, history of ovarian cyst |
| Mesenteric adenitis | High fever, generalized abdominal pain, tender enlarged lymph nodes may be palpable , recent upper respiratory tract infection |
| Intussusception | Bouts of abdominal pain with legs raised up, red current jelly stool, sausage shaped mass in abdomen |
What are the classical signs and symptoms which support the diagnosis of an acute appendicitis?
Periumbilical pain migrating to the right iliac fossa in the first 12-24 hours. Pain exacerbated on coughing ,moving( on speed bumps) may indicate peritoneum.
Also Anorexia, nausea, vomiting, low grade fever and Less frequently diarrhoea or constipation.
On Examination, Patient appears flushed, dehydrated with Low grade fever ,tachycardia
On abdominal examination there will be Right iliac fossa tenderness, Evidence of localized peritoneum such as guarding, rebound tenderness, percussion tenderness or Evidence of generalized peritonitis, generalized guarding and rigidity
There are some eponymous signs for appendicitis
- McBurney’s sign– deep tenderness over the McBurney’s point (1/3 rd distance from the anterior superior iliac spine to umbilicus)
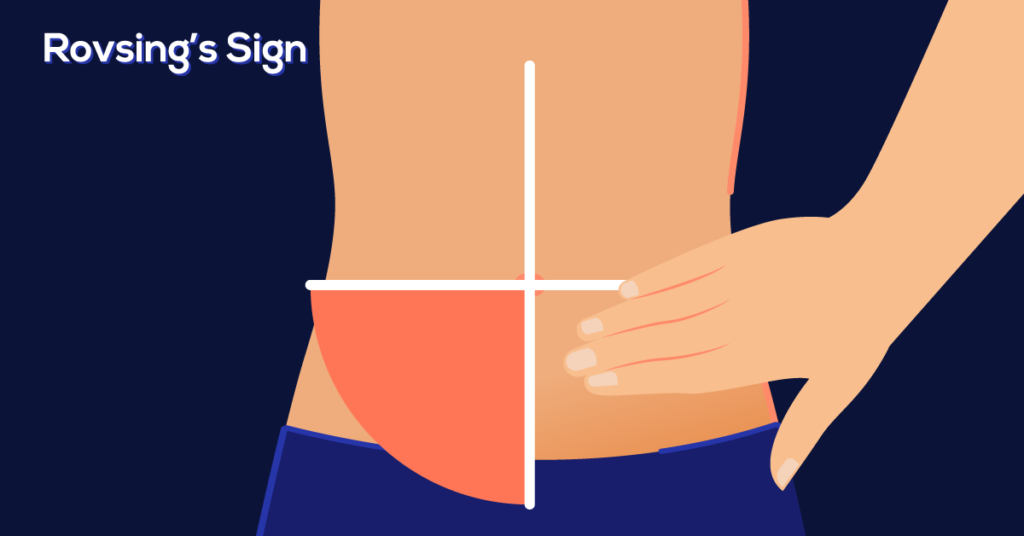
- Rovsing’s sign– Pain in the right iliac fossa on palpation of left iliac fossa
- Obturator sign– Pain on internal rotation of the right hip ( may indicate inflammation of a pelvic appendix)
- Psoas sign– Pain on full extension of the right hip( may indicate inflammation of a retrocaecal appendix)
- Dunphy’s sign- Increased pain in right iliac Foss with coughing.
Before moving on to the management let’s look at the anatomy of the appendix and how it causes migrating pain.
What is the Appendix?
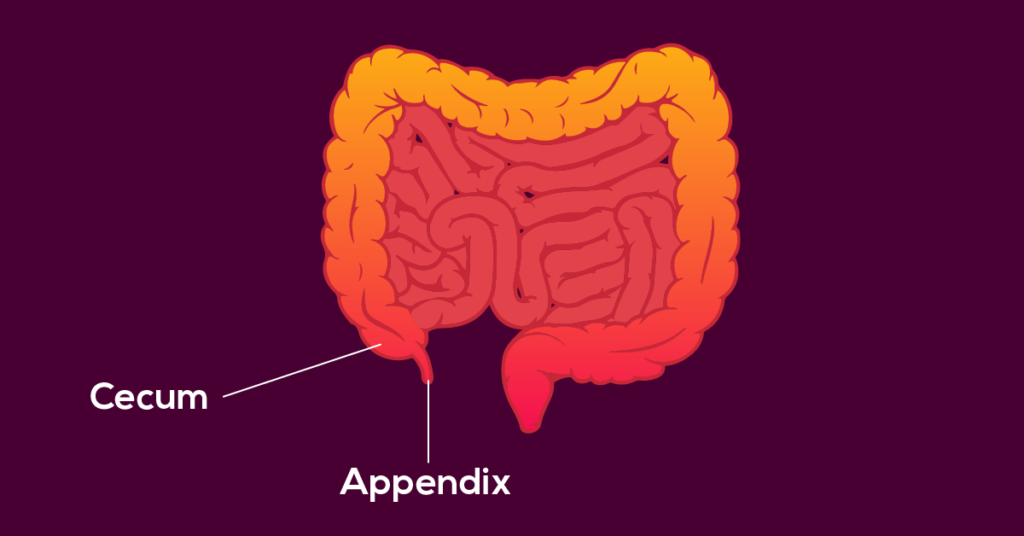
It is a narrow blind ending pouch approximately 5-9 cm long opening off the caecum. The base of the appendix is typically found 2.5 cm inferior to the ileocaecal valve, where the three taenia coli (longitudinal ribbons of smooth muscle) converge on the surface of the caecum at the posteromedial aspect.
It is a relatively mobile structure and may lie in a number of orientations. The commonest site is Retrocaecal appendix next Pelvic appendix. Other sites are Subcaecal appendix, Pre ileal and Post ileal appendix.
Blood supply by the Appendicular artery, a branch of the ileocolic artery derived from superior mesenteric artery. Nerve supply by autonomic nerves from superior mesenteric plexus.
What is this big mystery behind migrating pain?
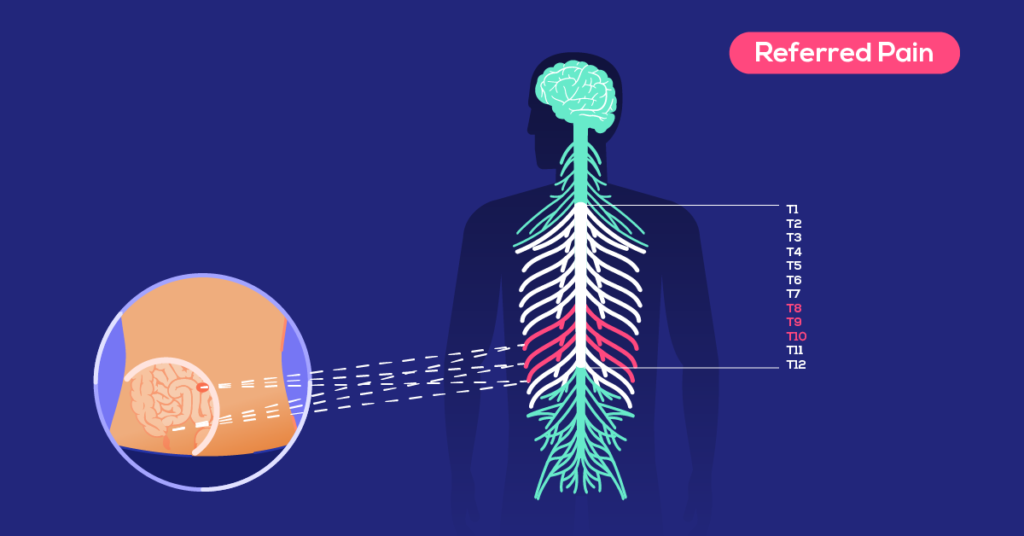
The appendix, along with the small bowel (distal to the ligament of Treitz), cecum, ascending colon, and 2/3 of the transverse colon are derived from the midgut. Pain in the midgut is primarily perceived via sympathetic afferents which comes from the 10th thoracic spinal segment(T10).
This T10 nerve root also supplies the T10 dermatome which innervates the Periumbilical region. Therefore initially when appendix is distended and stretched its pain is perceived as pain in Periumbilical region. This is called Referred pain.
With time when inflammation takes place and irritates the parietal peritoneum it gives rise to more localized pain as parietal peritoneum is supplied by somatic innervation, spinal nerves.
Investigations,
Appendicitis is mainly a clinical diagnosis. But investigations complement the diagnosis and help in excluding differentials.
Full blood count showing Neutrophil leukocytosis favors a diagnosis of acute appendicitis. There will be elevated C-reacted protein levels.
Urinalysis usually done to exclude UTI/ stones and Urine hCG test to exclude ectopic pregnancy.
Imaging;
X-ray abdomen is usually done to exclude other differentials. Not done in a clear case of appendicitis. USS abdomen- might show thickened ,inflamed appendix and free fluid in a case of perforation. It also can visualize perpendicular mass. CT is highly sensitive and specific for appendicitis, up to 98%, but is disadvantaged by its dose of ionizing radiation. It is widely used in older adults where appendicitis is less common and alternative diagnoses such as malignancy, right-sided diverticulitis or ischemic colitis should be considered.
Scoring systems,
There are a number of diagnostic scoring systems , although they are rarely used in practice. The more widely known are the Alvarado score, Paediatric Appendicitis score and Appendix Inflammatory Response score.
Management,
All most all the patients undergo the definitive treatment of Appendicectomy sooner or later. Every patient with suspected appendicitis should be admitted and managed with Analgesics, Anti emetics, IV fluids and Antibiotics. Patients with uncomplicated appendicitis can undergo Appendicectomy after the initial management. Patients with perforated appendix and peritonitis also undergo emergency Appendicectomy after initial resuscitation.
A non-operative strategy with antibiotics alone is favorable in some cases. It is most frequently considered in patients without generalized peritonitis or sepsis who have a significant operative risk, appendicular mass or active inflammatory bowel disease. Following a non-operative approach the appendix may be removed electively at a later stage once the infection has resolved, known as an interval appendicectomy. This is usually done 6-8 weeks later.
Appendicectomy,
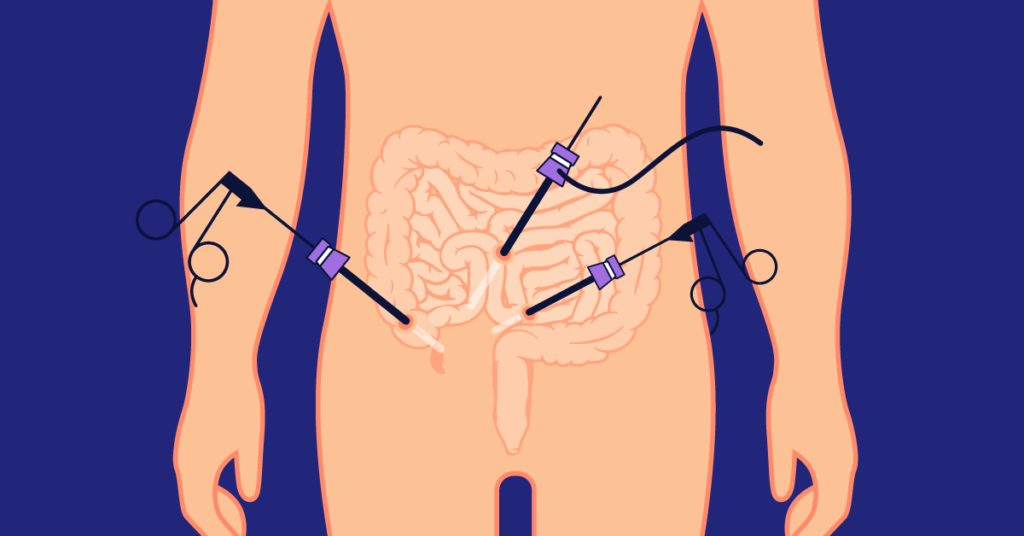
It can be done as an open surgery or laparoscopically. Laparoscopic Appendicectomy is becoming more common and in use with the wide availability of facilities. But still open appendicectomy is safe and remains widely used, particularly in small children, pregnancy, patients with severe cardiorespiratory disease unable to tolerate the pneumoperitoneum or patients with multiple previous surgeries where port access may be risky due to adhesions tethering bowel to the abdominal wall.
Open Appendicectomy is done via a small cut( Lanz incision) over the McBurney’s point. Appendix can be identified by tracing tenia coli from ceacum. Base of the appendix is where the 3 teania converges. In case of a peritonitis and perforation the incision has to be widened or need to be converted into a midline laparotomy to visualize the bowels and degree of contamination.
What would the surgeon do If the appendix appears normal intraoperatively?
Most surgeons will remove it if no other cause for the right iliac fossa pain is found; because 30% of macroscopically normal looking appendixes show signs of inflammation on histopathological examination. And it prevents the patient from having acute appendicitis in future and going for a repeated abdominal surgery.
Postoperative antibiotic management,
In simple non perforated appendicitis, post operative antibiotics should not exceed more than 24 hours. If there was a perforated appendicitis and significant intra abdominal contamination intravenous antibiotics should be Continued for 24-48 hours and a 5 day course completed. Antibiotics should be of broad spectrum with anaerobic coverage.
In Summary,
Appendicitis is a disease common in young. It has a short more acute disease course where the classic symptoms are migrating abdominal pain, nausea, vomiting, poor appetite with characteristic set of clinical signs. Diagnosis is mainly clinical. The mainstay of treatment is surgical removal of the appendix.
Q and A::
Is there a chronic appendicitis?
Sometimes patients can present with right lower quadrant pain for more than 5 days. When this occurs It Is that the appendix has ruptured and formed a appendicular mass or an abscess with surrounding tissue structures. It is usually managed medically with IV antibiotics. A large abscess is drained percutaneously.
What is Pseudoappendicitis?
Pseudoappendicitis refers to a disease which presents exactly like appendicitis but is due to another cause. The classic cause is a Yersinia enterocolitica infection which presents with right lower quadrant pain, fever, vomiting, and bloody diarrhea. Patients may have sick contacts. It is usually self- limiting , but in immunosuppressed patients can result in fatal sepsis. Treatment with doxycycline.
References,
- Surgery – A Case Based Clinical Review by Springer
- Bailey_&_Love’s_Short_Practice_of_Surgery_2018 27th edition
- Acute appendicitis by Hannah Sellars, Patricia Boorman – Intestinal surgery-11, Surgery International 35:8 2017. https://doi.org/10.1016/j.mpsur.2017.06.002
