Diabetes mellitus can be a very challenging disease to live with as it comes with a huge package of associated complications that can affect many vital organs inside the body. But on a positive note, most of these unfavorable outcomes can be either delayed or prevented altogether with simple acts of self-care.
For example, meticulous monitoring and regulating of blood sugar levels, proper medication, combined with healthy eating and healthy lifestyle can get you a very long way. But on the other hand, even simple acts of self-negligence can bring about grave outcomes and suffering.
Diabetic foot disease is one such serious complication of diabetes mellitus that can even deprive someone of the ability to stand on his/her own two feet. This condition is quite common all around the world.
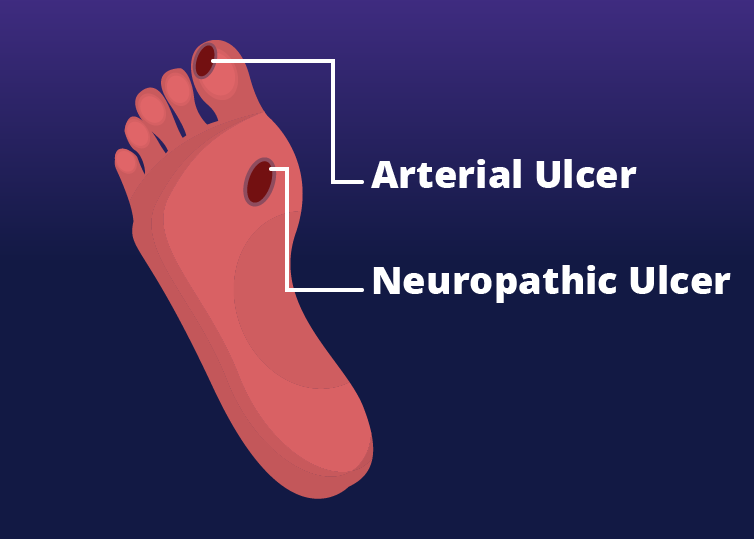
Data shows that nearly 6% of diabetic patients are prone to get diabetic foot diseases at some point or another.(1) This condition most of the time manifest as ulceration, infection, and tissue destruction of the foot.
Not only that, 85% of all amputations in diabetic patients are said to be the outcome of a foot ulceration which later gets complicated by severe gangrene (tissue death) or infection.(2) What is more upsetting is that about 0.03% and 1.5% of the affected individuals require amputation in order to save their lives.(3)
Table of Contents
What exactly causes the Diabetic Foot?
There are a few main culprits behind a diabetic foot. They are neurological, vascular, and immunological in origin; all relating to hyperglycemic state in a diabetic individual. Let’s look in detail how each one of these components result in diabetic foot disease.
Peripheral Neuropathy
Diabetes induces a state of hyperglycemia, or in other words, increased sugar levels within the body. This change can affect different cells of the body in different ways. (4)
- Hyperglycemia increases the oxidative stress on nerve cells, leading to a state of nerve dysfunction called neuropathy.
- Glucose molecules attach to proteins on nerve cells in a process called glycosylation, further increasing nerve cell dysfunction, on top of cutting off blood supply to the nerve cells resulting in ischemia. (low blood supply)
At the end, all these changes collectively start to manifest as motor, sensory, and autonomic complications of the diabetic foot that ultimately lead to ulceration.
When motor neurons supplying the musculature of the foot get damaged, it creates an imbalance between flexors and extensors of the foot. This marks the beginning of a series of unfavorable outcomes, that can lead to anatomical abnormalities of the foot.
Hammertoes, claw toes and Charcot neuroarthropathy (progressive destruction of the bones, joints, and soft tissues) are few such abnormalities which occur in the foot that could eventually lead to ulcer formation.
In addition, any damage to the autonomic nerves supplying the foot could impair the function of sweat glands in the skin. As a result, the skin can get drier since its ability to moisturize is not functioning properly anymore. This increases the occurrence of epidermal cracks and skin breakdown, which in turn could easily give rise to the formation of skin ulcers.
Not only that, diabetic patients often tend to lose peripheral sensations, especially in the foot, which means, there’s a chance that the patient could be unaware of any ulcers already existing on the foot, simply because he/she doesn’t feet its existence in the first place. When someone actually start noticing it, the foot could even be beyond salvageable.
Vascular Changes
Peripheral arterial disease as a result of hyperglycemic state is another major causative factor for diabetic foot disease. When increased blood sugar levels remain elevated for a long period of time it causes changes in the arteries of the peripheries, especially in the limbs.
These changes include endothelial dysfunction and smooth muscle abnormalities of the walls of the peripheral arteries. As a result, reduced vasodilation and increased constriction of the artery lumen can occur.(5)
When the blood supply is either reduced or cut-off to the lower extremities, it results in ischemia and increased risk of ulceration in diabetic individuals.
Immune Changes
Proper functioning of the immune system including T-lymphocytes is also important in the wound healing process. Study data shows an increased rate of apoptosis of T-lymphocytes in patients with non-healing chronic foot ulcers.(6)
Diagnosing Diabetic Foot Disease
If you are suffering from diabetes mellitus for quite for some time now, you must be curious to know for sure whether you already have diabetic foot disease or you are simply at risk of getting it someday near in the future.
A thorough foot examination is the key to detecting the disease early. In addition, a history of ulcers, amputations along with poor glycemic control would obviously hint at something similar happening again.
Let’s look at some clinical findings that would indicate the presence of diabetic foot disease;
- Presence of any ulcers or areas of gangrene (dead tissue) indicating the presence of an active, ongoing disease.
- Presence of skin lesions such as cracks and skin fissures, deformed nails, macerated web spaces, calluses and evidence of fungal infections.
- Presence of foot deformities such as hammer toes, claw toes, and pes cavus that could increase the risk of getting the disease.
- Feeling numbness, tingling, or pain in the foot indicating nerve damage.
- Presence of a cold foot might indicate lack of blood supply or ischemia.
- Increased warmth in the foot along with swelling and redness might point towards the presence of inflammation such as cellulitis or acute Charcot foot.
- Looking sick and unwell, with or without fever, in addition to changes in respiration and blood pressure might indicate a more serious life-threatening complication of the ulcer like sepsis.
Tests to diagnose
The Monofilament Test is used to detect peripheral neuropathy in diabetic individuals. This test tries to identify patients who have reduced sensations and hence lost their sense of protection in the feet.
This test uses a monofilament which exerts a 10 g force as it bends. If an individual fails to sense a 10 g pressure, that particular individual is considered to be without the protective sensation.
On the other hand, in order to detect peripheral arterial disease, a hand-held Doppler device is used to calculate the ankle-brachial index, which indicates how severely affected the peripheral arterial blood flow is.
What makes you more prone to getting diabetic foot disease?
Although, technically anyone with diabetes mellitus can get diabetic foot disease, there are certain factors that puts you at more risk than others.(7)
- Having very poor glycemic control with very high blood sugar levels.
- Having diabetes mellitus for a very long duration.
- Having high blood pressure
- Being overweight
- Having a high lipid profile
- Being more than 40-years of age
How can you prevent diabetic foot disease?
As the popular saying goes; “prevention is always better than cure”. Same can be said for the diabetic foot disease as well. There are a few simple things that everyone can do to prevent having a nasty diabetic ulcer on your foot.
· Maintain adequate glycemic control
Controlling your blood sugar levels from the very beginning makes you a very strong candidate in the fight against diabetic foot disease. Maintaining optimal blood sugar levels and serum glycated hemoglobin (HbA1c) levels in the body is really important. It’s only by then that the prevention of the disease or delaying the disease progression can be achieved.
However, achieving good glycemic control does not mean you could completely reverse neuropathy which has already begun to set in. It only allows you to avoid any further damages from occurring.
· Undergo regular foot examinations
For individuals with low-risk of diabetic ulcers, annual foot assessments are recommended. For those who belong to the mid-risk and high-risk categories, more frequent assessments are encouraged.
According to the recommendations of the International Working Group on Diabetic Foot (IWGDF) classification diabetic foot screening by a medical professional must be carried out(8);
- Once each year for diabetic patients without peripheral neuropathy
- Every six months for those who already have peripheral neuropathy
- Every 3 to 6 months for individuals with peripheral neuropathy, in addition to having peripheral arterial disease and/or foot deformity
- Every 1 to 3 months for those who are with peripheral neuropathy and already having a history of previous ulceration or amputation in the lower extremity
However, even without medical inspection for the presence of pedal ulcers, there are simple everyday things we all can practice which might actually be useful in identifying early signs of ulcers or even better, in preventing them from occurring in the first place. Now, let’s look into some of those useful tips that could come in handy in maintaining good foot hygiene in diabetic individuals.
Useful tips on foot care for people with diabetes mellitus
- Make sure to inspect your feet daily. Look for calluses, skin cuts, redness, swelling, blisters or any nail changes. Do not forget to check the area between two toes. Get the help from someone else if you find it difficult to inspect properly. Making use of a mirror is another great option.
- Wash your feet daily. Make use of water at room temperature for washing. Avoid soaking feet as much as possible. Do not forget to dry your feet properly after washing, especially, between the toes.
- It is okay to use creams or any other lubricant for dry skin, but make sure to avoid applying any them in the space between toes.
- Trim your nails straight across without cutting into the two ends. If you find it difficult to reach them and do it on your own, get help from someone else. The best time to cut your nails is after bathing, as it is when the nails are the softest. You can smooth them with a nail file. Make sure not to cut the cuticles.
- Try not to walk barefoot at all times. You never know when you will step on something that will injure your foot. Always better to take the simple precautionary measures.
- Wear socks with your shoes and make sure that they are dry. And do not forget to inspect the inside of the shoes for any kind of foreign body, before putting them on. Avoid socks that are either too loose or too tight. Loose socks can create friction inside the shoes, while tight socks tend to cut-off adequate blood circulation.
- Never try to remove calluses on your own at home, especially using a chemical agent or plaster. It is better to get help from a trained individual like a podiatrist.
- Exercising regularly and engaging in foot strengthening exercises or stretches. Being immobile can cause stiffness in your feet musculature and other tissues around. Therefore, it is important to keep them mobile and flexible. You can even try air drawing letters with your toes, when you keep your feet up at your leisure time.
- Quit smoking and eat healthy food items. This will reduce the risk of peripheral arterial disease and help you maintain your glycemic control.
- Wear appropriate footwear. When your shoe is too tight and your foot is crammed inside, it increases the risk of your foot getting injured due to something or another. Not to mention, tight footwear can increase the risk of fungal infection with too much sweating inside.
Make sure that your toes have adequate space inside your shoe to move around freely. The shoe should be at least half an inch longer than your longest toe and wide enough for your foot.
Ideally, shoes for diabetic individuals should have soft-cushioned soles, a wide toe box, laces for adjustment, and an extra room inside to accommodate orthosis if required.
Individuals with ulcers at the forefoot or the heel are prescribed a special type of offloading footwear to allow room for ulcer healing. They reduce the pressure on a specific part of the foot. They also prevent the risk of recurrence.
When should you seek medical attention?
- When there is cramping or pain in your lower limbs, especially burning, tingling-type of pain in the feet.
- When your feet feel numb or you start to experience reduced sensations than before.
- Any change in temperature of the feet; too warm or too cold
- Change in color; either pale or red
- Loss of hair on the surface of the lower limb
- Presence of a sore, ulcer, callous, ingrown toenail or a blister
- Evidence of a fungal infection in your nails
- Any visible change in the shape of your foot
Individuals with poorly controlled diabetes are at the highest risk of developing diabetic foot disease and associated complications.
Most of these grave outcomes can be easily prevented with a good understanding and adherence to proper foot care and other lifestyle modifications. For those who are with advanced diabetic foot disease, optimal wound care practices are essential to prevent any further serious complication like amputations.
Therefore, there’s no doubt that providing proper education regarding foot care to both patients and caregivers alike and implementing them accordingly is quite crucial in winning this particular battle against the diabetic foot disease.
References
1. Zhang P, Lu J, Jing Y, Tang S, Zhu D, Bi Y. Global epidemiology of diabetic foot ulceration: a systematic review and meta-analysis†. Vol. 49, Annals of Medicine. Taylor and Francis Ltd; 2017. p. 106–16.
2. Lepäntalo M, Apelqvist J, Setacci C, Ricco JB, De Donato G, Becker F, et al. Chapter V: Diabetic foot. Eur J Vasc Endovasc Surg [Internet]. 2011 Dec [cited 2021 Feb 6];42(SUPPL. 2). Available from: https://pubmed.ncbi.nlm.nih.gov/22172474/
3. Lazzarini PA, Hurn SE, Fernando ME, Jen SD, Kuys SS, Kamp MC, et al. Prevalence of foot disease and risk factors in general inpatient populations: A systematic review and meta-analysis. BMJ Open [Internet]. 2015 [cited 2021 Feb 6];5(11). Available from: https://pubmed.ncbi.nlm.nih.gov/26597864/
4. Aumiller WD, Dollahite HA. Pathogenesis and management of diabetic foot ulcers. J Am Acad Physician Assist [Internet]. 2015 May 1 [cited 2021 Feb 6];28(5):28–34. Available from: https://journals.lww.com/01720610-201505000-00006
5. Clayton W, Elasy TA. A review of the pathophysiology, classification, and treatment of foot ulcers in diabetic patients [Internet]. Vol. 27, Clinical Diabetes. American Diabetes Association; 2009 [cited 2021 Feb 7]. p. 52–8. Available from: https://clinical.diabetesjournals.org/content/27/2/52
6. Arya A, Garg S, Kumar S, Meena L, Tripathi K. Estimation of lymphocyte apoptosis in patients with chronic, non healing diabetic foot ulcer. Int J Med Sci Public Heal. 2013;2(4):811.
7. Diabetes and Your Feet | Diabetes | CDC [Internet]. [cited 2021 Feb 7]. Available from: https://www.cdc.gov/diabetes/library/features/healthy-feet.html
8. Schaper NC, Van Netten JJ, Apelqvist J, Lipsky BA, Bakker K. Prevention and management of foot problems in diabetes: A Summary Guidance for Daily Practice 2015, based on the IWGDF guidance documents. Diabetes Res Clin Pract [Internet]. 2017 Feb 1 [cited 2021 Feb 7];124:84–92. Available from: https://pubmed.ncbi.nlm.nih.gov/28119194/
